
If you’ve worked in the medical field, you’ve had a day in the clinic that was scary, for one reason or another. And just like in horror movies, there are different kinds of scary. There are experiences that shock you, gross you out, or leave you with a sense of impending doom. You might even receive an unexpected phone call. In the spirit of Halloween, we asked Quintessence authors to share their scary cases with us. If you read this article after dark, you might want to keep the lights on.
Cranial Fracture
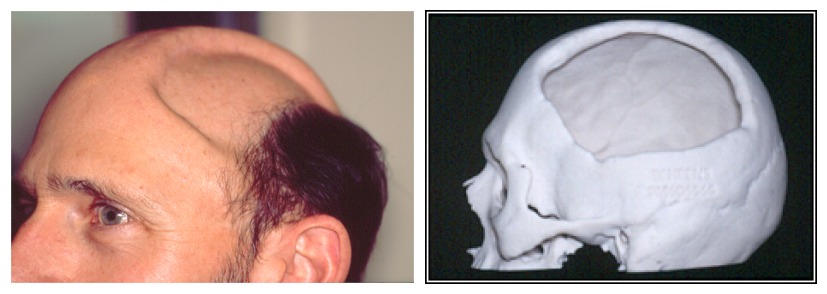
Our first case is from Dr Johan Reyneke, author of three editions of Essentials of Orthognathic Surgery. This patient, a 46-year-old man who was a dentist himself, sustained a cranial fracture after a cycling accident. The fracture developed an infection, resulting in sequestration of the outer table of his cranium. On examination, the inner cranial bone was found to be mobile, putting the brain in jeopardy. Dr Reyneke was able to correct the defect by using a 3D computer-generated model and creating a patient-matched implant. He used a unilateral coronal approach to place the implant, resulting in a full recovery and renewed confidence for the patient.

Hepatic Carcinoma Metastasis
Dr Paul Coceancig remembers a bloody case from his first day of work: “I was in Singapore General Hospital in the oral surgery clinic. It was my first day on the job. I was called by a very anxious dental nurse, who pulled me into the dental office of my new and very pale junior colleague who had an 80-year-old—and extremely pale—patient with literally a liter of bright red blood around his boots. My colleague had just done a mucosal biopsy of what turned out to be a hepatic carcinoma metastasis that had lodged inside the cheek as a bright red blister. They apparently bleed without any chance of control, but that’s not something anyone knew at the time.
Without really spending much time to think about it, I jumped right in with a huge stitch that curved around the mandible to compress the facial artery that was supplying the area in question. My buddy was patting me on the back, shaking my hand, and the old bloke was starting to pink up. But then my senior colleague—the one who ran the clinic—walked in, saw all the blood, and cut the stitch that was tied over the skin as it wasn’t ‘intraoral.’ I didn’t have time to say ‘NOOOOO!’
The bleeding immediately restarted, and nothing she did seemed to work, until she too asked for the same stitch to be retied, so I stepped right back in.
We all learned something that day.”
Severe Dental Trauma
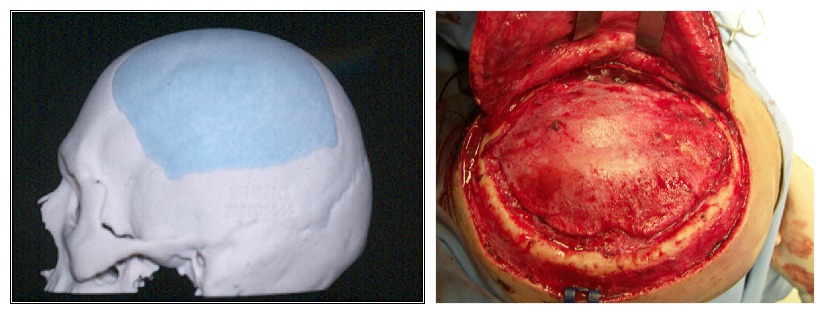
Dr David Sarver looks back on a challenging case of a patient who experienced severe dental trauma and serious bodily injury, which is also featured in his new book Dentofacial Esthetics: From Macro to Micro: “Emergencies don’t often happen with orthodontics, but this one rattled me a bit. This 24-year-old woman was referred to me after being struck by a car while living abroad. She had recovered from her fractured limbs and ribs, and now it was time to take care of her teeth, which had been stabilized with a bonded fiber strip.
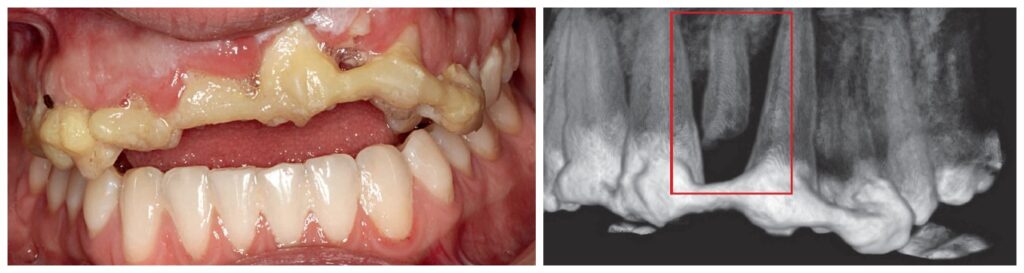
It was hard to see what I was looking at with all the acrylic and gingival hypertrophy (Fig 1), so I took a CBCT scan to see what was under there. Most of the tooth crowns and roots were intact, but some were avulsed and/or fractured (Fig 2). My first thought was that all of these traumatized teeth would have to be extracted, because saving them would certainly be impossible. But then I considered the bony defect and cascade of effects that would follow, a fate I wanted to avoid for this young woman. Instead, my goal was to preserve as much bone as possible. It was worth a try to save whatever I could.
“The story certainly didn’t end here, but the scary part was over.”—Dr Sarver
After administering local anesthesia, I gently removed the bonded splint and all the bonding material, and then I used a diode laser to remove all the hypertrophic gingiva (Fig 3). Full fixed appliances were placed, and within 6 weeks the maxillary anterior teeth were almost in contact with the mandibular incisors, and the CBCT showed intact roots that, surprisingly, were asymptomatic (Fig 4). No teeth were lost on my watch, and the patient had the stability she needed to continue restorative treatment. The story certainly didn’t end here, but the scary part was over.”

Hereditary Gingival Fibromatosis
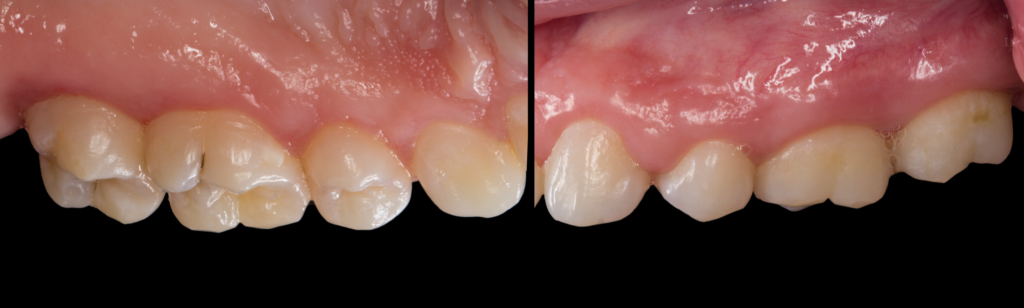
Dr Gustavo Avila-Ortiz sent us some before and after photos of this case of hereditary gingival fibromatosis, a very rare periodontal condition treated with gingivectomy. Very scary for someone who’s never encountered it before!

Vampire Dentist
Dr Daniel Ninan, author of Dentistry and the Pregnant Patient, recalls an otherworldly experience: “When I was working as a mobile dentist, I went to a facility to see a patient. The patient was very nice. However, when I entered the patient’s room, the other person in the room held up a cross and kept the cross between me and them. I wondered if she perhaps thought I was a vampire.”
Face-Eating Incident
Remember the face-eating incident in Miami in 2012? Yoh Sawatari, DDS, author of Surgical Management of Maxillofacial Fractures, was the facial trauma attending who got the initial call that day, and to this day he remembers the call he received from the intern: “Sawatari, I have a patient who had his face eaten by another person, what do you want me to do?” As he was contemplating his career choices, he got a call from the director of trauma: “Plastics wants to take the case, do you mind?” Dr Sawatari didn’t mind at all.

Thank you to the Quintessence authors who shared their scary cases with us! Be sure to check out their books to learn more about how to treat cases, whether they’re scary, routine, or somewhere in between. Happy Halloween!
