Reading time: 11 minutes
Imagine yourself as a beginning dental student. You attend your first restorative dentistry conference where you hear the term treatment planning. Intrigued and eager to learn how to develop a plan of care for your future patients, you pull out your notebook, pen poised over the page. But by the end of the conference, you’re still no clearer on the concept than when you arrived. Disheartened, you return to school. A year later, the subject has only been touched on briefly in your classes, always within the context of a specific discipline. By the time you’re walking down the aisle with your diploma, nothing has changed. You know all the details but are still unsure how to put them all together.
Treatment planning is implied but never formally taught.
According to Antonio H.C. Rodrigues, CD, CAGS, MScD, a basic understanding of treatment planning is a common problem his students face. In fact, it’s something even experienced dentists struggle with. He defines treatment planning as “giving a solution to a previously identified problem.” The Glossary of Prosthodontic Terms further defines the concept as “a sequence of procedures planned for the treatment of a patient after diagnosis.” In other words, the problem (ie, diagnosis) dictates the solution (ie, treatment).
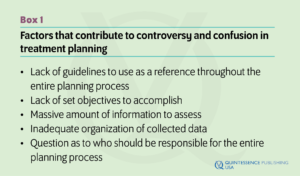
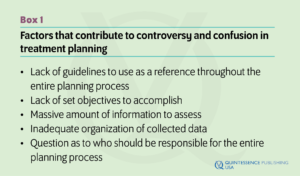 Successful treatment planning requires intimate knowledge and understanding of the problem, the solution, and any treatment modifiers, which is part of the philosophy of comprehensive care that Dr Rodrigues practices. While treatment planning is a vital part of overall treatment and crucial for long-term success, the process of how to effectively plan a treatment often remains vague and confusing due to the lack of available education. Dental schools are bereft of courses exclusively dedicated to the subject, yet it is too basic a topic to be covered at most scientific conferences. Treatment planning is implied but never formally taught. This oversight in education, coupled with tomes of literature too specialized to be helpful, leaves inexperienced practitioners floundering and overwhelmed.
Successful treatment planning requires intimate knowledge and understanding of the problem, the solution, and any treatment modifiers, which is part of the philosophy of comprehensive care that Dr Rodrigues practices. While treatment planning is a vital part of overall treatment and crucial for long-term success, the process of how to effectively plan a treatment often remains vague and confusing due to the lack of available education. Dental schools are bereft of courses exclusively dedicated to the subject, yet it is too basic a topic to be covered at most scientific conferences. Treatment planning is implied but never formally taught. This oversight in education, coupled with tomes of literature too specialized to be helpful, leaves inexperienced practitioners floundering and overwhelmed.
“While much has been written on treatment planning, most authors tend to concentrate their thoughts within their own specialty,” Dr Rodrigues explains. “Consequently, only a segmented view of the patient’s condition is presented, which may compromise treatment results in the long term.”
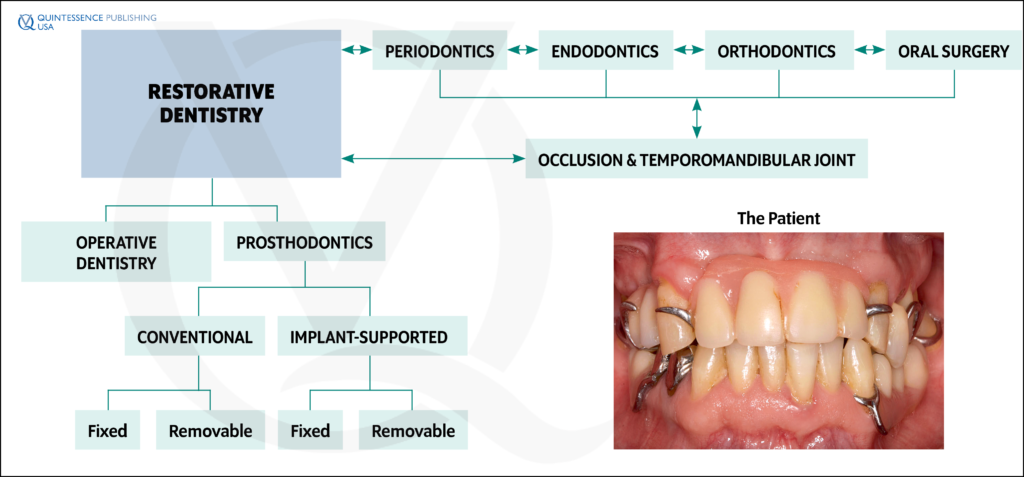
The book encompasses treatment planning beyond the specialty, which stresses the importance of cultivating relationships with other specialties to make the best recommendations to meet patients’ needs.
Because there are no set guidelines in planning procedures, students find themselves grappling with endless questions on how to sift through the information to determine what’s important, how to decide what to do first, and how to pull it all together. After observing his students resort to the fickle insights of intuition, Dr Rodrigues developed a comprehensive resource called Treatment Planning in Restorative Dentistry and Implant Prosthodontics. The first of its kind, his book provides a way to systematize the process so it’s not left to a scattershot approach. The need for this philosophy of total care is high due to the current emphasis on predictability, reliability, and successful long-term results.
“My book provides a comprehensive approach to treatment planning, outlining a clear, objective, and simple thinking process that can be easily applied in daily practice,” Dr Rodrigues says. “It essentially provides the reader with a roadmap to be used as a reference from the very initial procedures until the final restorative treatment, always considering the patient in his or her entirety.”
In the past, discussions between different areas of expertise were discouraged in favor of quick solutions, but it’s crucial for clinicians to think beyond their own skillset to maximize treatment success. The book encompasses treatment planning beyond the specialty, which stresses the importance of cultivating relationships with other specialties to make the best recommendations to meet patients’ needs.
History of Treatment Planning
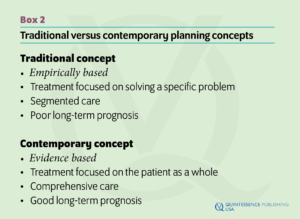
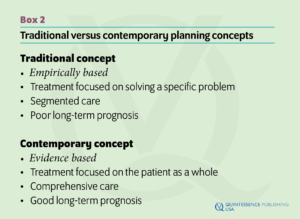
The early days of treatment planning called for brief, quick-hit discussion and immediate recommendation to arrive at a simple solution. This decision was often shrouded in uncertainty and based on the dentist’s empirical experience, without any scientific evidence behind it. The diagnosis was not clearly articulated, especially not to the patient. Furthermore, the patient was not provided with treatment options and usually left treatment decisions up to the dentist’s personal judgment.
“Most complications and failures, particularly in restorative dentistry, are directly or indirectly related to inadequate planning.”
The intent was to solve a specific problem in a specific area, often based heavily on patient request. This led to cases of treatments tailored to patient expectations without further analysis to investigate other potential problems. The result of such segmented care was an inefficient, often detrimental treatment that caused more problems for the patient in the long run.
“Most complications and failures, particularly in restorative dentistry, are directly or indirectly related to inadequate planning,” Dr Rodrigues stresses. “When planning procedures are not carried out accordingly, dentists tend to provide either overtreatment or undertreatment for their patients. Either situation may cause problems in the long term. Therefore a book offering guidelines to help the dentist with the development of predictable planning procedures is of utmost importance.”
“Comprehensive planning is the planning approach that considers the patient as a whole as opposed to the individual specialty planning which focuses mainly on a specific area or problem.”
With Treatment Planning in Restorative Dentistry and Implant Prosthodontics, the previous norm of a short discussion of limited treatment possibilities has been replaced with an open format of informed, in-depth conversations about every realistic solution within the range of available treatment options. Gone are the days of specific problem solving without consideration for the larger context, which led to significant problems being overlooked. Dr Rodrigues urges clinicians to focus on comprehensive patient care to achieve long-term success. In other words, they should make sure the treatment plan is complete before considering specialty options.
“Comprehensive planning is the planning approach that considers the patient as a whole as opposed to the individual specialty planning which focuses mainly on a specific area or problem,” Dr Rodrigues says. “Both planning modalities are of paramount importance for achieving successful results. However, before treating a specific area or problem, the dentist should first become familiar with the patient in his or her entirety.”
Philosophy of Comprehensive Care

Phases of the treatment planning protocol and their requisite procedures: (1) gathering and organization of clinical data and development of the problem list; (2) interpretation of the gathered data and determination of the diagnosis, prognosis, and treatment objectives; (3) analysis of the treatment options and development of the treatment plan; and (4) patient education, treatment plan presentation, and informed consent.
The philosophy Dr Rodrigues practices and advocates for consists of three parts:
- A comprehensive approach to treatment planning
- Restorative planning principles
- The planning process
Executing a comprehensive approach involves keeping all the patient’s dental needs in mind while assessing the vast amount of data necessary to make a plan. Thorough clinical extraoral and intraoral examinations are key for collecting this data. Treatment Planning in Restorative Dentistry and Implant Prosthodontics provides numerous forms to ease data entry and analysis, including examination checklists and questionnaires, problem lists, and treatment plan outlines. The extraoral examination encompasses the head and neck while the intraoral examination covers the entire oral cavity using diagnostic aids, including radiographs; diagnostic casts, wax-ups, and indices; radiographic templates; and clinical photography.
Standardization is important to promote efficiency and facilitate training, so Dr Rodrigues advises that clinicians perform examinations using the same sequence every time. While they may initially adapt the sequence to their unique practice, he recommends the following sequence for the extraoral examination: (1) face as a whole (ie, facial and dentofacial analysis) and (2) mouth (ie, smile analysis). He also recommends the following intraoral examination sequence: (1) oral mucosa, (2) periodontium, (3) teeth, (4) occlusion and TMJs, (5) edentulous areas, (6) possible orthodontic needs, and (7) possible major oral surgery needs. Teeth should first be evaluated individually, then as a group. The recommended individual tooth sequence is as follows: (1) crown, (2) pulp chamber, (3) root canal, (4) lamina dura, and (5) periodontal ligament space from occlusal surface to apex. Intraoral examinations require an assistant to serve as secretary for data input.
Following data collection, there are three principles of restorative planning to consider: (1) making a diagnosis based on the patient’s current state of health, (2) envisioning the patient’s healthy state, and (3) comparing the two. The first principle involves the clinician’s ability to evaluate the patient’s current state and diagnose the problem accordingly. The second principle is to envision the patient’s healthy state and distinguish between acquired problems and congenital problems. The third principle involves comparing the first two principles to develop a plan to return to the normal healthy state.
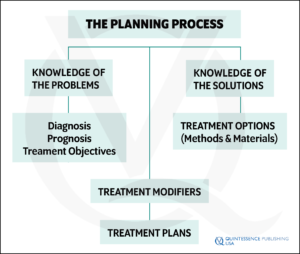
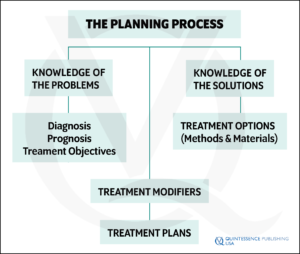
Elements involved in the planning process.
The final part of the philosophy involves asking what, how, and who. First, clinicians must develop a firm grasp of what treatment planning is. Then they must understand how to treatment plan. This means outlining the objectives that planning procedures should achieve. In the past, treatment planning existed simply to arrive at a plan of action for generating a general treatment outline and formal payment agreement. Today’s treatment plans go one step further by serving as a valuable patient education tool and reliable means of obtaining informed consent.
The dentist’s role has shifted from final authority to expert advisor, and a major goal of ethical contemporary dentistry involves adequately preparing patients to make sound health care decisions in their best interest. This translates to fully informing patients about their individual conditions and outlining all methods available for treatment. Evidence-based decision-making is an essential part of the process, so it is important for clinicians to supplement the discussion with evidence from dental literature and results from their own practices. Clinicians should identify all existing problems or factors that may lead to problems and weigh the benefits and prognosis of each option. The goal of the treatment plan presentation is to relay all findings, including any scientific information necessary for the patient to make an assessment. With that goal in mind, the core objectives of contemporary treatment planning involve developing a total treatment plan, promoting patient education, and obtaining informed consent.
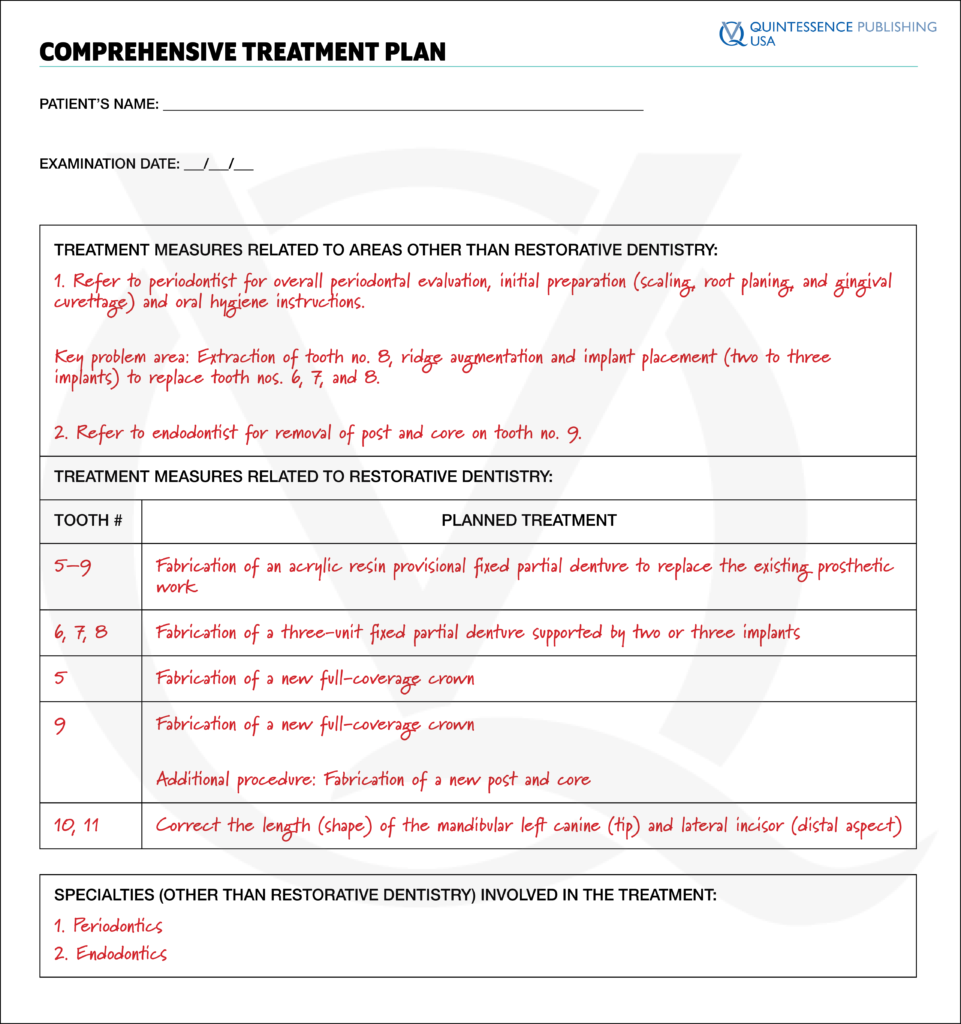
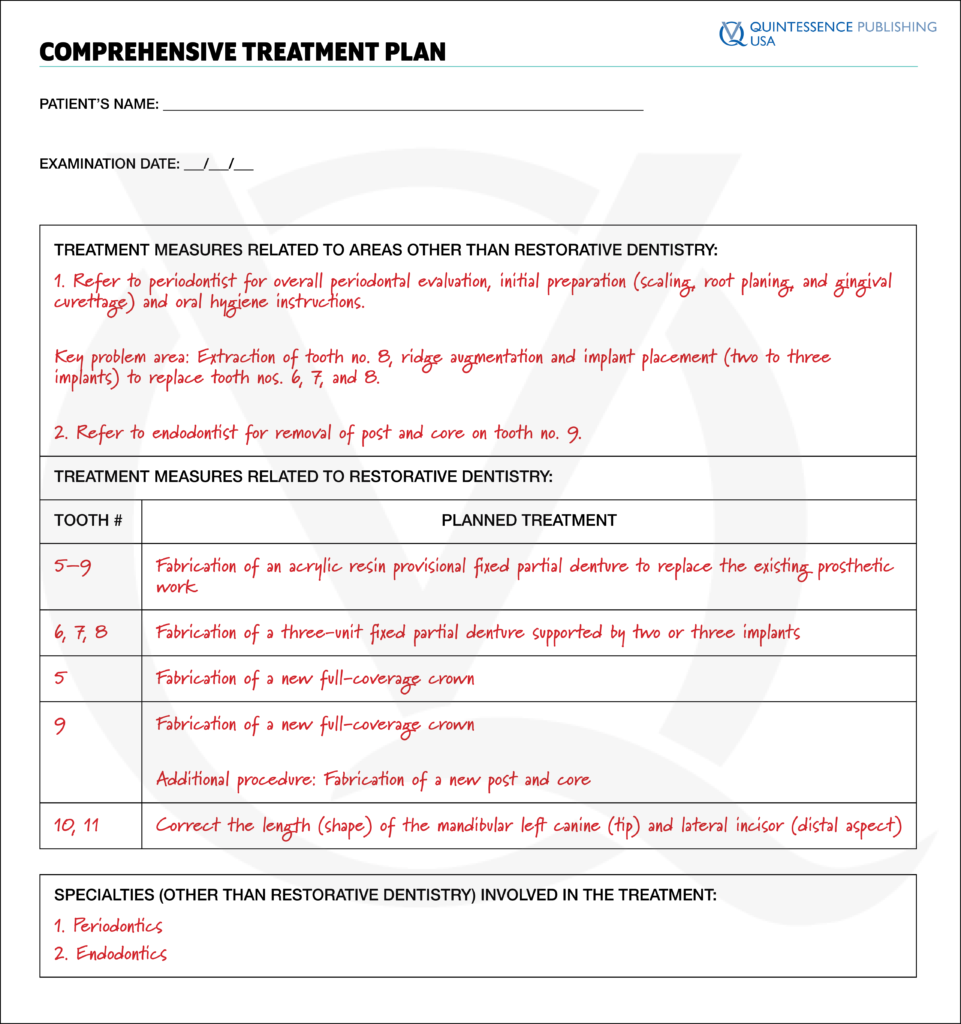
Sample comprehensive treatment plan.
Finally, clinicians must understand who is best positioned to oversee the treatment from beginning to end. There is often disagreement on which specialty to manage the planning process, but Dr Rodrigues believes this role is ideal for the clinician who delivers the restorative therapy. By developing a solid treatment plan, this person is responsible for preparing the patient to make the best treatment choice. Therefore, it is the duty of the treatment planner to maintain clear, organized notes and to make consultations and necessary referrals to other specialists as needed.
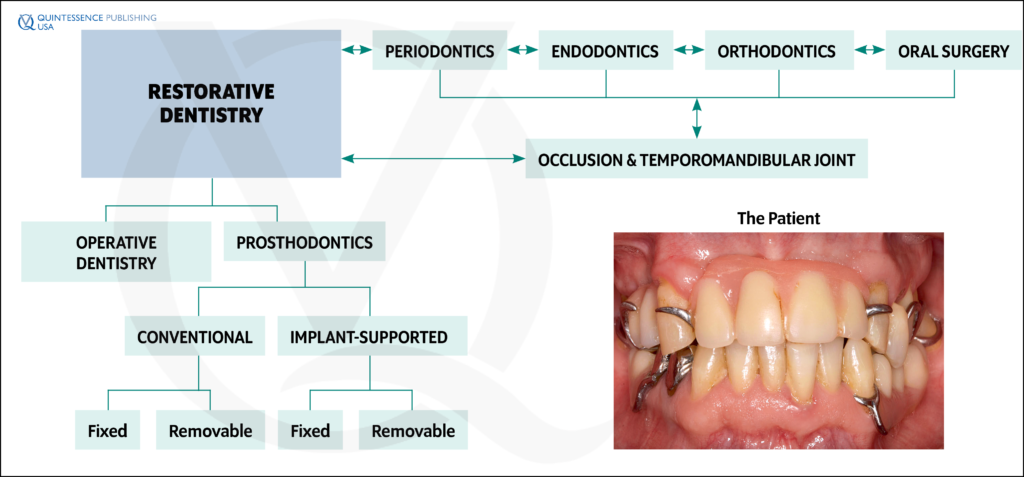
Diagram showing all areas involved in the development of a comprehensive plan of treatment.
“A philosophy providing a thought process to be used in all situations, combined with a consistent and methodical approach, would definitely increase both reliability and predictability in long-term results of the dental treatment as a whole.”
“In view of contemporary dentistry, making a diagnosis and planning a treatment implies the professional responsibility to omit nothing of consequence for the patient,” Dr Rodrigues says. “Deviation from this line of thought has become unacceptable and is no longer tolerated. Therefore, there is a distinct need to teach dental students and all professionals involved with restorative procedures to fulfill their responsibility in the management of a comprehensive treatment plan for the patient, and there has long been a need for an efficient method to successfully address this issue. A philosophy providing a thought process to be used in all situations, combined with a consistent and methodical approach, would definitely increase both reliability and predictability in long-term results of the dental treatment as a whole.”
 Antonio H.C. Rodrigues, CD, CAGS, MScD, was trained in prosthodontics at Boston University School of Dental Medicine and holds a Master of Science degree in prosthodontics. He is an associate professor at the Catholic University of Minas Gerais School of Dentistry in Belo Horizonte, Brazil, where he is the clinical coordinator of the Graduate Division of Conventional Prosthodontics and Implant Prosthetics. He is a former adjunct associate professor in the Division of Postdoctoral Prosthodontics in the Department of Restorative Sciences and Biomaterials at Boston University Goldman School of Dental Medicine, where he continues to lecture on a regular basis. Dr Rodrigues has lectured extensively in Brazil, the United States, and Europe. He has been involved with many research projects, and his written contributions include articles in conventional and implant prosthodontics. Dr Rodrigues has maintained a private practice limited to prosthodontics and operative dentistry for more than 30 years.
Antonio H.C. Rodrigues, CD, CAGS, MScD, was trained in prosthodontics at Boston University School of Dental Medicine and holds a Master of Science degree in prosthodontics. He is an associate professor at the Catholic University of Minas Gerais School of Dentistry in Belo Horizonte, Brazil, where he is the clinical coordinator of the Graduate Division of Conventional Prosthodontics and Implant Prosthetics. He is a former adjunct associate professor in the Division of Postdoctoral Prosthodontics in the Department of Restorative Sciences and Biomaterials at Boston University Goldman School of Dental Medicine, where he continues to lecture on a regular basis. Dr Rodrigues has lectured extensively in Brazil, the United States, and Europe. He has been involved with many research projects, and his written contributions include articles in conventional and implant prosthodontics. Dr Rodrigues has maintained a private practice limited to prosthodontics and operative dentistry for more than 30 years.
 Treatment Planning in Restorative Dentistry and Implant Prosthodontics
Treatment Planning in Restorative Dentistry and Implant Prosthodontics
Antonio H.C. Rodrigues
Treatment planning is commonly considered one of the most important phases of any dental treatment and vital for achieving successful long-term results. However, most dental schools do not offer courses exclusively designed for comprehensive planning, and comprehensive planning is rarely discussed at scientific meetings because it is considered a basic topic that practitioners should already understand. This knowledge gap leaves practicing clinicians with few options beyond using their own intuition to solve problems, which is highly unpredictable. Therefore, this book presents clinical guidelines for planning treatments in restorative dentistry and outlines a clear, objective, and simple thinking process that can be easily applied in daily practice, essentially providing the reader with a roadmap to be used as a reference from the very initial procedures until final restorative treatment. Part 1 describes how to identify existing problems by gathering, organizing, and analyzing information obtained during clinical examination. Examination checklists and forms are included to ensure that no important information is left out during the evaluation process. Part 2 focuses on providing solutions to identified problems via restorative treatment options, highlighting the use of implant-supported restorations in the treatment of both partially and completely edentulous arches. Part 3 details how to present treatment options to the patient and includes aspects related to patient education, treatment plan presentation, and obtaining informed consent from the patient. Altogether, this book will transform the way you treatment plan your cases.
320 pp; 1,100 illus; ©2020; ISBN 978-0-86715-826-7 (B8267); US $168
Contents
1. Rationale for Developing a Philosophy of Total Care
Part One
2. Gathering and Organizing Clinical Data: Initial Consultation
3. Gathering and Organizing Clinical Data: Clinical Examination
4. Extraoral Examination
5. Intraoral Examination: Soft Tissues
6. Intraoral Examination: Hard Tissues
7. Intraoral Examination: Edentulous Areas
8. Intraoral Examination: Specialty Considerations
9. Interpreting the Collected Data, Determining the Diagnosis and Prognosis, and Establishing Treatment Objectives
Part Two
10. Restorative Treatment
11. Conventional Restorative Dentistry
12. Implant-Supported Restorations
13. Treatment Plan Development
Part Three
14. Preparing the Patient to Make an Informed Decision
This article was written by Sarah Mondello, Quintessence Publishing.
©2019 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO PART MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER.
 Aesthetic Dental Strategies: Art, Science, and Technology
Aesthetic Dental Strategies: Art, Science, and Technology Piezoelectric Bone Surgery: A New Paradigm
Piezoelectric Bone Surgery: A New Paradigm Tooth-Preserving Surgery
Tooth-Preserving Surgery Dentofacial Esthetics: From Macro to Micro
Dentofacial Esthetics: From Macro to Micro