When Ken Berley, DDS, JD, first began practicing dentistry, sleep-related breathing disorders (SRBDs) were not on his radar. He didn’t realize how deadly SRBDs could be for his patients, and he didn’t know he should be screening for them. One fateful event, though, would change the course of both his life and his professional career.
“When I received the phone call from my mother, everything changed,” Dr Berley recalls. “I remember the night like it was yesterday. The phone rings at 2:00 am, and through sobs I hear my mother say, ‘Ken, your father has had a stroke.’ I can still remember the panic in her voice. For the next 48 hours, my father lay in a coma, and I sat at his bedside watching him struggle to breathe. We had been informed that the stroke was massive and there was little hope. He was having one apneic event after another, and finally he passed away.”
What Dr Berley and his father’s physicians did not know at the time was that all of the men in the Berley family were predisposed to obstructive sleep apnea (OSA) and that 90% of the time strokes are caused by OSA. The loss of his father set several gears in motion, and Dr Berley began to make connections between his family history and current research on sleep and strokes.
“I come from a family of big men,” Dr Berley explains. “My grandfather was 6’4″ and 270 lbs back when men were never that big. When my father had his stroke, he weighed over 280 lbs. I was raised in a small house in Arkansas with thin walls separating our bedrooms. After all these years I vividly remember the many nights I was unable to sleep due to the snoring that was blaring through those walls. I was amazed that my mother was able to sleep in the same room. Dad was a champion snorer! I would love to know what decibel levels he was able to hit while he was in full snore. Of course, 50 years ago the seriousness of sleep-disordered breathing was completely unknown. We simply accepted snoring as a normal result of being ‘Berley’ men.
“When my grandfather passed away from a stroke in the middle of the night, everyone in my family was thankful that he died in his sleep as there was no prolonged illness or suffering. ‘God was good to him’ was repeated throughout the funeral. With time, my grandfather’s passing became a distant memory. The fact that he died in his sleep and was a horrific snorer did not register in my brain. However, when my father died the same way, everything came into focus. One stroke during sleep might have been a coincidence, but two could not be ignored. I started learning everything I could about how snoring was related to strokes during sleep. That quest led me to my commitment to the study and treatment of snoring and OSA.”
What are SRBDs?
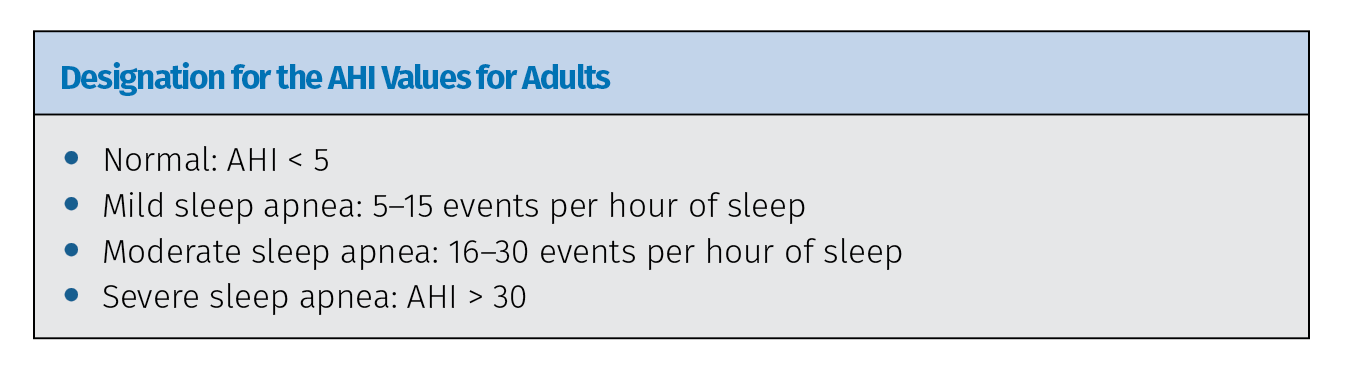
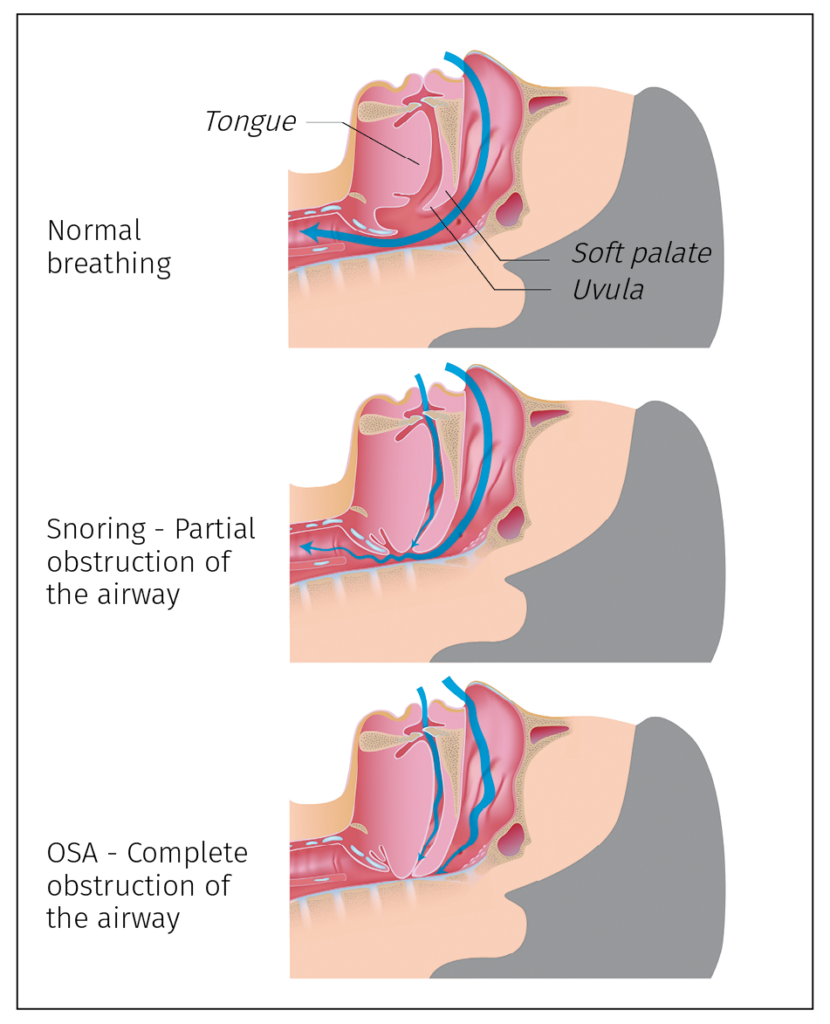
Sleep-related breathing disorders, or SRBDs, are chronic diseases caused by repeated upper airway collapse during sleep. The class includes a range of breathing anomalies, with OSA being the most recognized and most serious of the known SRBDs. OSA is characterized by repetitive episodes of partial or complete obstruction of the patient’s airway during sleep, despite the effort to breathe, and is usually associated with a reduction in blood oxygen saturation. Repetitive reduction of airflow is called hypopnea, and complete cessation of airflow is termed apnea. These episodes of decreased breathing, called apneas (literally meaning “without breath”), typically last 20 to 30 seconds. The level of OSA is described by the Apnea-Hypopnea Index (AHI), which is a count of respiratory events divided by the time of testing. A patient’s AHI is derived using a polysomnogram (PSG), or sleep study, which measures several physiologic aspects to determine the quality of a patient’s sleep. PSGs record changes in brainwaves, eye movements, muscle tone, heart rate, leg movements, and respiration. A sleep physician then reviews the data recorded by the PSG, identifies any anomalies, and makes the appropriate diagnosis.

Prevalence of SRBDs and sleep apnea syndrome, according to age and sex, as reported by the HypnoLaus Study in 2015. (a) A mild SRBD was defined as between 5 and 14 events per hour, while severe SRBD was defined as at least 30 events per hour. SRBD categories differed by age (P < .0001 in men and in women). (b) Mild sleep apnea syndrome was defined as between 5 and 14 events per hour and an Epworth score greater than 10, moderate sleep apnea syndrome was defined as between 15 and 19 events per hour and an Epworth score greater than 10, and severe sleep apnea syndrome was defined as at least 30 events per hour and an Epworth score greater than 10. Categories of sleep apnea syndrome differed by age (P < .0001 in men and P < .001 in women).
OSA is largely an anatomical problem. The physical characteristics of the human airway that make complex vocalization possible—our flexible upper airway and suspended mandible—also place us at risk for OSA. During sleep, muscle tone decreases, which can allow inspiratory pressure to collapse into the airway during sleep. The mandible and hyoid bones are suspended, allowing the tongue, soft palate, uvula, and epiglottis to collapse into the airway, creating a complete or partial obstruction superior to the thyroid cartilage and inferior to the hard palate in susceptible individuals. Added risk comes from the fact that, as humans have evolved, the human cranium has increased in size and capacity while the craniofacial respiratory complex has decreased in size. As a result of the smaller oral cavity, the tongue has been progressively displaced posteriorly into the airway, a problem that is exacerbated during sleep. The collapsible nature of the upper airway coupled with a narrow maxilla, small mandible, and displaced tongue has placed humans at great risk for airway obstruction. These anatomical issues can be exacerbated by obesity because as patients become larger, fat deposits in the base of the tongue and the lateral walls of the airway enlarge as well. It is estimated that 70% of OSA sufferers are obese.
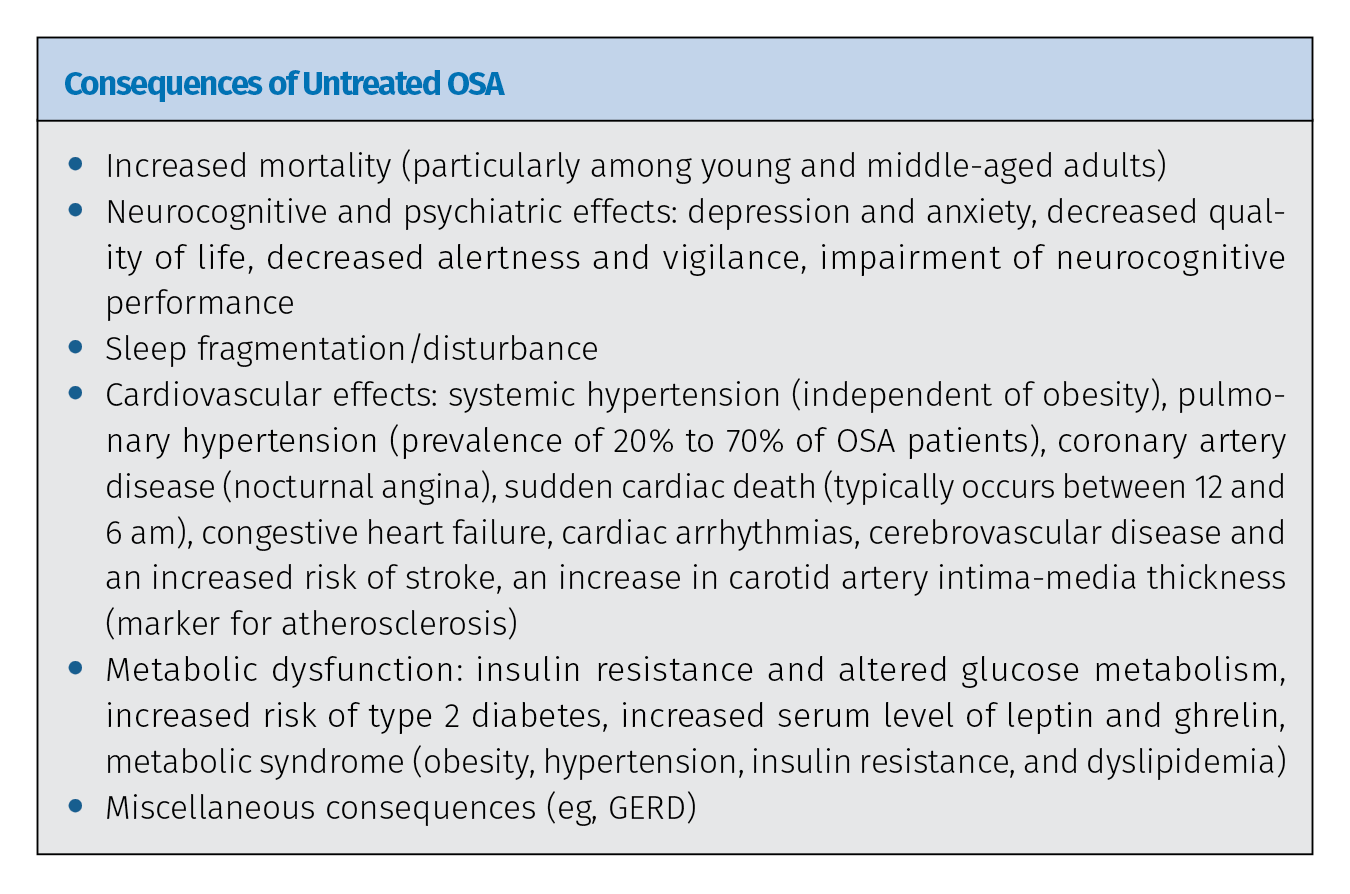
OSA can be deadly. In patients with OSA, hypoxia during apneic episodes results in a sympathetic response and the release of cortisol, initiating the fight or flight response and contributing to sleep disruption and daytime sleepiness. Additionally, the carotid bodies, a small cluster of chemoreceptors and supporting cells located near the bifurcation of the carotid arteries, detect changes in the oxygen/carbon dioxide composition of arterial blood. A decrease in the partial pressure of oxygen and increase in partial pressure of carbon dioxide activates the sympathetic nervous system, which causes the patient’s heart rate to elevate, blood pressure to increase, and respiratory effort to increase. The effect of these sympathetic episodes is an increase in chronic disease and shortened life expectancy in untreated OSA patients.
The majority of individuals with sleep disorders do not present to the physicians for treatment of their sleep issues, but many of these patients will present for routine dental examination and care. A dentist who is properly trained can provide life-saving referrals.
“All dentists must become knowledgeable in the treatment and screening of sleep disorders,” adds Dr Berley, who also uses his extensive law knowledge and experience to advise clinicians on developing their dental sleep medicine practices. “The new ADA statement on the role of dentists in the treatment of SRBDs states that dentists should be screening for OSA, meaning screening for SRBDs will be the standard of care for dentists within a short period of time. From a legal perspective, once the ADA issued the policy statement of the role of dentists in the treatment of SRBDs, plaintiffs’ attorneys will utilize that policy statement as a learned treatise in court to establish a standard of care. Also, I am currently working with several state boards of dentistry to establish their own policy statements that are in line with the ADA. Therefore, within a short period of time, dentists will be legally responsible for conducting a screening during each examination to check for airway insufficiency.”

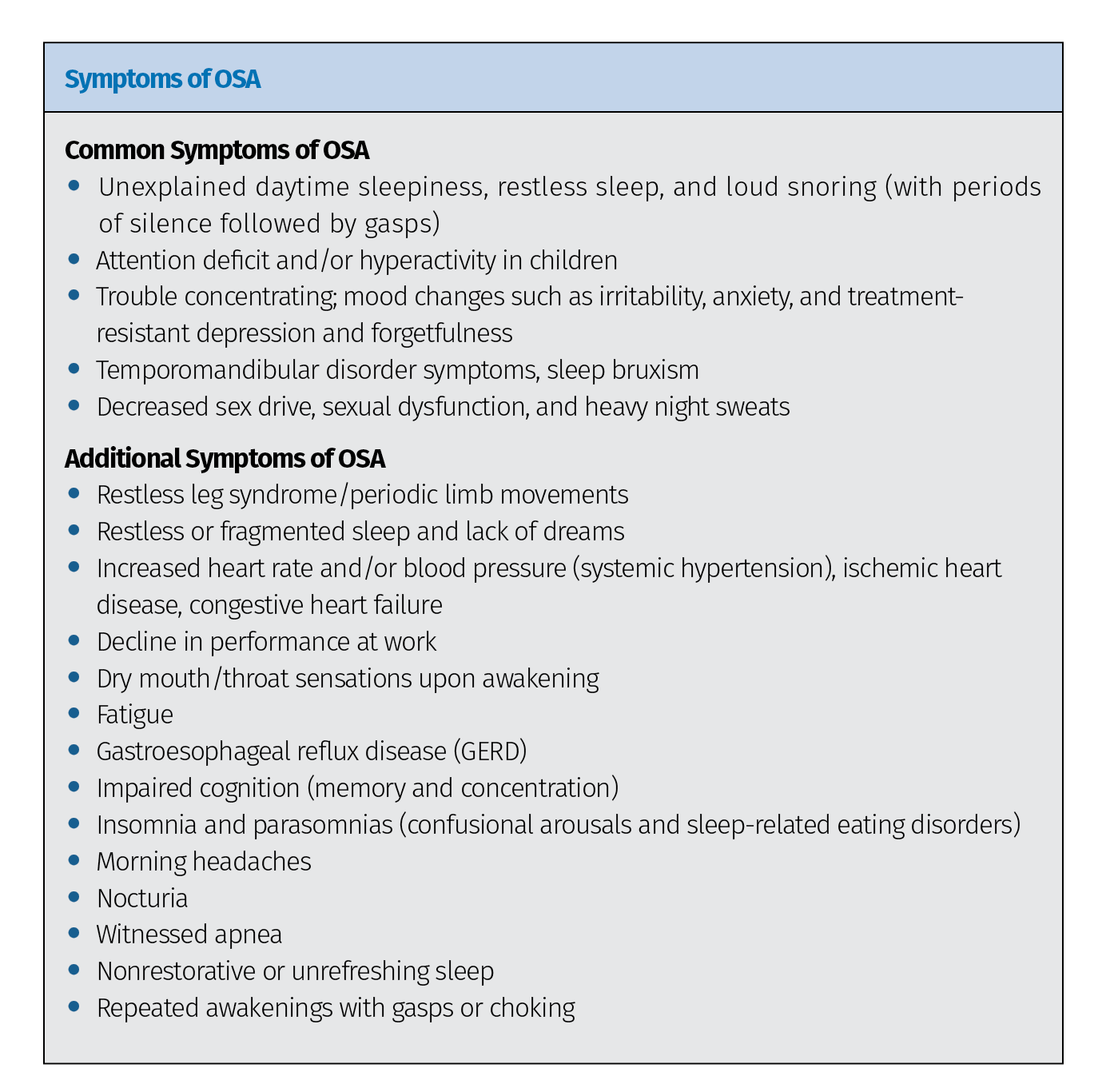
Adapted from Ramar et al.
“Dentists are in a unique position to change the lives of millions of patients,” Dr Berley continues. “Statistics show that dentists routinely evaluate approximately 50% of the American population each year. It is estimated that 24% of adult men, 9% of adult women, and 10% of children in the US suffer from OSA, and it is estimated that 80% to 90% of all patients who suffer from this devastating disease remain undiagnosed. It is also estimated that each dental office in the United States may have as many as 500 or more patients with undiagnosed OSA currently being treated for dental-related concerns. Therefore, dental professionals have never been presented with a better opportunity to positively impact the health of our patients, but studies have consistently shown that many dentists are unable to recognize systemic and oral risks of OSA. This educational deficiency must be corrected.”
Treating OSA: How Dentists Can Be Involved
The current therapy of choice for OSA is continuous positive air pressure (CPAP) therapy. CPAP works by administering a constant and continuous stream of air under pressure through a mask that is worn over the nose or nose and mouth. The pressure is set to prevent collapse in the oropharynx from negative respiratory pressure and can be customized. When used, CPAP is the most effective means of preventing closure of the airway and thus reducing AHI. But adherence to the therapy is a big problem.
“There are many reasons why people don’t use CPAP,” Dr Carstensen explains. “Each person chooses for themselves how they will think about their diagnosis and the medical risk it poses for them. They have social reasons to pursue therapy, but any medical treatment that requires their cooperation also demands their commitment. If they don’t believe in the value for themselves, overcoming the troublesomeness of the therapy is going to be a problem. The biggest problem in adherence to CPAP therapy isn’t the device—it’s the patient deciding that the benefit does not outweigh the cons. Recent research has found that patients with low levels of certain SRBDs and mild symptoms are far less likely to adhere to CPAP therapy. Reasons people report to me for not using CPAP include the hassle factor of putting the mask on, discomfort from the mask and straps, air flowing into their eyes, complaints by their bed partner, and the inconvenience of traveling with the CPAP machine. Air being pushed into their stomach, drying of their mouth, noise from the machine, and claustrophobia are other frequent issues.”
Each person chooses for themselves how they will think about their diagnosis and the medical risk it poses for them.
Medicare considers a patient to be compliant with CPAP when it is used 4 hours per night at least 5 nights per week. But if a patient sleeps 8 hours per night, 7 nights per week, then a patient using CPAP for 20 out of 56 total hours of sleep in a week—less than half!—is still considered compliant. Additionally, many studies report ranges as low as 25% full compliance over 1 year. SRBDs can be deadly, so a lack of adherence to CPAP therapy is a serious issue, both on an individual basis for each patient and in the broader scheme of how successful sleep medicine can be in treating conditions like OSA.
Enter dentists. CPAP therapy is the medical solution to OSA; oral appliance therapy (OAT) using a mandibular advancement device (MAD) is the dental solution. MADs prevent obstruction of the airway by advancing the mandible, and with it the tongue, thereby expanding the upper airway. Additionally, while it is being worn, the MAD holds the mandible in a stable position throughout the night. Because they are anchored by the teeth for stability, dentists alone are qualified to treat SRBDs using these devices.
Studies have consistently shown that many dentists are unable to recognize systemic and oral risks of OSA. This educational deficiency must be corrected.
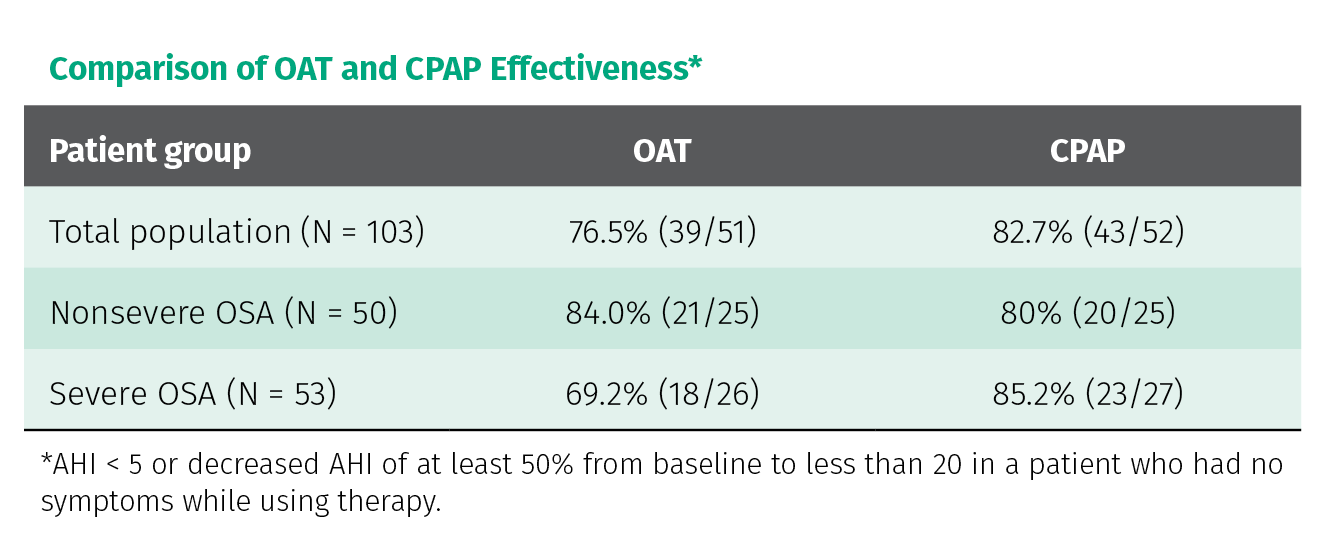
So how well does OAT with a MAD work when compared with CPAP?
The treatment the patient will use is always more valuable than the one they reject.
“There is more and more research showing that while CPAP therapy is more effective at reducing patient AHI, MAD therapy is more acceptable to more patients,” Dr Carstensen adds. “Physicians and researchers are becoming increasingly aware that the lowest possible AHI is not the only target and that the treatment the patient will use is always more valuable than the one they reject. CPAP therapy is not superior to MAD therapy for many other respiratory details that can be measured, so as the scope of attention widens beyond the most basic measurements, MAD therapy is becoming more accepted for more patients.”
So how did the two patients mentioned above fare when MAD therapy was offered instead of CPAP? The young woman’s AHI was reduced to 1.2, and the MAD was accepted by her boyfriend. The other patient’s AHI was reduced to 0, and his sinus infections completely stopped.
The longest REM sessions occur in the second half of the night, meaning that patients who remove the CPAP midway through the night frequently face the most serious stages of sleep unprotected.
“With the medical records from the sleep physician came a prescription for an oral appliance,” he continues. “Susan was happy to move forward and was soon accommodated to the device, which she immediately felt was better than her CPAP. We did send her home with monitors to refine her jaw position, but we were able to achieve a normal AHI and eliminated all flow limitations within 8 weeks of meeting her. Her subjective symptoms completely resolved once we had her jaw postured correctly. She was absolutely thrilled we were able to reach this positive outcome so quickly, contrasting it with her 3-year trial of CPAP therapy, and she was a little annoyed that her sleep physician didn’t suggest this in the first place.”
The treatment plan also doesn’t have to be an either/or decision with clinicians choosing between the advantages of MAD therapy or the advantages of CPAP therapy, weighed against the disadvantages of both.
“For patients who are religiously trying to comply with CPAP but are unable to wear their device all night,” Dr Berley explains, “we can provide a MAD to be worn in conjunction with CPAP. We call this combination therapy. In this situation, the oral appliance is placed in the mouth, then the CPAP is positioned. The MAD helps open the patient’s airway so that the pressure setting on the CPAP can be reduced below what it would need to be set at without the MAD, thereby making the CPAP easier to wear. This provides the patient with the best possible outcome. The oral appliance is typically left in place even if the CPAP is removed during the night, meaning the patient still has a level of protection. Additionally, the MAD can be used in times of power outages and off-the-grid situations.”
Dr Carstensen gives an example of this treatment plan in practice: “April was referred from a physician after a sleep lab experience. The test showed severe OSA, so, as was the order, the sleep technologist woke April to place a CPAP and see if that could help her. The mask lasted fewer than 30 seconds, and April left the room immediately. She said, ‘I’d rather die in my sleep than use that mask.’ We made her a well-fitted, well-tolerated oral appliance that, sadly, was not effective enough at controlling her OSA. I needed her to be able to use a CPAP, probably in combination with the oral device, so I referred her to a sleep-aware psychiatrist who helped April get past some PTSD issues that were triggering her CPAP aversion. Afterward, April became a new person. She felt great, had a better frame of mind, and was happily using her CPAP device most nights and her oral appliance on weekends and for traveling. She could not have achieved this excellent health outcome without a team of involved providers willing to find the right solution for her rather than focusing only on their own areas of expertise. It was rewarding knowing that I facilitated this happy outcome—an experience that was uncommon in most restorative dentistry cases.”

(a and b) Herbst appliance. (c) EMA appliance. (d) dreamTAP appliance. (e) ProSomnus [IA] appliance. (f) Dorsal fin appliance. (g) ProSomnus [CA] appliance. (h) Moses appliance.
Working with Our Partners in Medicine
So how do you dive in? Dental sleep medicine is a growing field of dentistry, but the amount of ‘new tricks’ to learn has kept many dentists from stepping out of their comfort zone. In addition to the learning curve that applies to implementing any new form of treatment, dental sleep medicine is also uniquely challenging in that it involves careful cooperation with a board-certified sleep physician. Because OSA is considered a medical disease, dentists cannot legally diagnose it. The PSG testing and diagnosis instead must come from a sleep physician; after diagnosis, treatment either comes from the sleep physician by way of CPAP therapy or, with physician referral, treatment with OAT from a trained dentist. It’s a complicated dance between the fields of medicine and dentistry, but dentists shouldn’t feel overwhelmed. The path is possible, and, in fact, the junctions with medicine actually offer some advantages to dentists.
“Because OSA is a medical condition,” Dr Berley explains, “OAT is filed on the patient’s medical insurance. There are no dental codes available. This presents a major opportunity to provide OAT and not utilize your patient’s dental insurance benefits. The treatment of OSA with MADs can also provide an additional income stream for offices wishing to expand their services. Many practitioners who provide OAT are routinely billing medical insurance for payment. All diagnosis and treatment planning for SRBDs/OSA is provided by a sleep physician, who controls the treatment and determines when OAT is appropriate for a patient, then refers that patient to a dentist for OAT.”
Dentists trained in dental sleep medicine can be a vital member of a multidisciplinary team of health care professionals working together to control this deadly disease.
“SRBDs directly or indirectly affect many biologic systems within the human body,” Dr Berley explains. “Therefore, numerous medical disciplines are involved in the treatment of OSA comorbid conditions. This fact has allowed dentists to develop an extensive physician-based referral practice. Dentists trained in dental sleep medicine can be a vital member of a multidisciplinary team of health care professionals working together to control this deadly disease.”
There’s a lot to learn before you break into dental sleep medicine. To both help and encourage fellow dentists to get involved, Drs Berley and Carstensen have coauthored The Clinician’s Handbook of Dental Sleep Medicine, which effectively serves as a comprehensive how-to manual for starting a dental sleep medicine practice. All of the information clinicians need is covered: the current scientific knowledge of SRBDs, the clinical information needed to provide and deliver OAT, guidance for filing OAT on a patient’s medical insurance or Medicare, and the legal information necessary for navigating a complicated system at the boundary of dentistry and medicine.
“What I want is for every dentist to be aware of SRBDs, look for them in their practice, and facilitate a solution for them,” Dr Carstensen states. “I grew up with my father being an epic snorer, thinking nothing about it in connection with health. With my knowledge now of airway, snoring, sleep apnea, and the effects of these problems, I don’t want dentists to think their family members and patients are simply snorers. My father has severe sleep apnea; after I finally got him to a sleep doctor, he began using a CPAP device and enjoyed his most productive years at work in the few remaining before retirement. After retiring, he was able to drive safely around North America in his RV for the next 17 years. If our book helps clinicians decide that they can treat patients like my father, they can share the rewards that come from truly making a difference in these patients’ lives. This positive work will generate rewards in their own lives, as well.”
“While I love to lecture and show the amazing clinical results of OAT, the real joy is hearing the stories of how our therapy changes the lives of our patients,” Dr Berley adds. “My favorite story is of one of the first patients I treated. He was 32 years old when he was first diagnosed. He was an athletic young man whom you never would have dreamed was a severe apneic, but he had a very small oral cavity secondary to four orthodontic premolar extractions. His AHI was 54, and he snored like a freight train. While the snoring was inconvenient, it never caused him many problems—until he got engaged. Suddenly, the snoring was the most important thing in his life. Shortly after he was married, he was in trouble. He was tested for OSA and placed on CPAP. He tried desperately to comply with CPAP treatment, but to no avail. Within 6 months of being married, he was relegated to the guest bedroom, and the couple was in marriage counseling. The wife could not understand how difficult it can be for some patients to comply with CPAP. After OAT, his AHI was reduced to 0.4, but—more importantly—his snoring completely stopped. The couple now has three children, and the wife will personally call me to let me know when I need to adjust her husband’s appliance.
“My journey of study into OSA culminated in two things,” Dr Berley concludes. “As a patient, my journey led me to the Herbst appliance that I wear each night. As a clinician, my journey led me to The Clinician’s Handbook of Dental Sleep Medicine. I hope my experience gives readers a small glimpse into the satisfaction of providing OAT for the treatment of SRBDs, and I hope our book gives clinicians the courage to start their own journeys. Had it not been for the introduction of dental sleep medicine into my practice protocol, I would have retired several years ago. Treating OSA has made dentistry fun again. If you’re looking for something to reinvigorate your passion for dentistry, take a good look at dental sleep medicine—you will not be disappointed. And if there is anything I can do to assist you, please feel free to contact me.”
 Ken Berley, DDS, JD, is a dentist and lawyer who, for the past 10 years, has focused his dental practice on the treatment of sleep-disordered breathing and temporomandibular disorders. He is also the president of a consulting firm offering in-office training on dental sleep medicine (DSM) and consent forms and documents to assist the DSM practice. Dr Berley is a Diplomate of the American Board of Dental Sleep Medicine and regularly lectures in the areas of risk management and the development of a successful DSM practice. He has been published in Sleep Review magazine and other journals associated with sleep-disordered breathing, and he provides consulting services for various insurance companies and actively defends and advises dentists who are facing legal challenges.
Ken Berley, DDS, JD, is a dentist and lawyer who, for the past 10 years, has focused his dental practice on the treatment of sleep-disordered breathing and temporomandibular disorders. He is also the president of a consulting firm offering in-office training on dental sleep medicine (DSM) and consent forms and documents to assist the DSM practice. Dr Berley is a Diplomate of the American Board of Dental Sleep Medicine and regularly lectures in the areas of risk management and the development of a successful DSM practice. He has been published in Sleep Review magazine and other journals associated with sleep-disordered breathing, and he provides consulting services for various insurance companies and actively defends and advises dentists who are facing legal challenges.
 Steve Carstensen, DDS, started treating sleep problems in 1998 and maintains a private practice in Bellevue, Washington. He has completed a Mini-Residency in Sleep at the University of California, Los Angeles, and is a Diplomate of the American Board of Dental Sleep Medicine. He lectures internationally, directs sleep education at the Pankey Institute, and is a guest lecturer at Spear Education, University of the Pacific, and Louisiana State University Dental Schools. Since 2014, he has been editor-in-chief of Dental Sleep Practice Magazine.
Steve Carstensen, DDS, started treating sleep problems in 1998 and maintains a private practice in Bellevue, Washington. He has completed a Mini-Residency in Sleep at the University of California, Los Angeles, and is a Diplomate of the American Board of Dental Sleep Medicine. He lectures internationally, directs sleep education at the Pankey Institute, and is a guest lecturer at Spear Education, University of the Pacific, and Louisiana State University Dental Schools. Since 2014, he has been editor-in-chief of Dental Sleep Practice Magazine.
 The Clinician’s Handbook for Dental Sleep Medicine
The Clinician’s Handbook for Dental Sleep Medicine
Ken Berley and Steve Carstensen
It has been estimated that 20 million Americans suffer from moderate to severe OSA, and at least one patient in five has mild OSA. The primary treatment prescribed by sleep physicians is CPAP, but patient compliance with this therapy is unacceptably low, between 25% and 50%. There is a significant opportunity for dentists to provide a viable alternative therapy—oral appliance therapy (OAT). OAT results in much better adherence to therapy than CPAP, and while OAT is not as efficacious as CPAP, this increased compliance results in comparable therapeutic results. Currently, a board-certified sleep physician is the only medical professional qualified to diagnose OSA and other sleep-related breathing disorders (SRBDs), so dentists must coordinate with a sleep physician to provide OAT. This book is the how-to guide, a gateway to a successful dental sleep medicine practice. Written by two experts in the field, it clearly delineates the dentist’s role in the treatment of SRBDs and gives practical advice for how to incorporate dental sleep medicine into an existing dental practice, not to mention how to work with sleep physicians to best support patient care. In addition to step-by-step instructions for examination, appliance selection, and follow-up care, complications of OAT, legal issues, and medical insurance and Medicare considerations are included to fully prepare the dentist for the journey into dental sleep medicine.
240 pp (softcover); 60 illus; ©2019; ISBN 978-0-86715-813-7 (B8137); Now available! $72
This article was written by Caitlin Davis, Quintessence Publishing.
©2019 BY QUINTESSENCE PUBLISHING CO, INC. PRINTING OF THIS DOCUMENT IS RESTRICTED TO PERSONAL USE ONLY. NO PART MAY BE REPRODUCED OR TRANSMITTED IN ANY FORM WITHOUT WRITTEN PERMISSION FROM THE PUBLISHER.








 Dr Richard J. Miron is currently Visiting Faculty in the Department of Periodontology at the University of Bern in Switzerland, where he completed his PhD studies. He has published over 150 peer-reviewed articles and lectures internationally on many topics relating to growth factors, bone biomaterials, and guided bone regeneration. Dr Miron has been awarded many top international prizes in regenerative dentistry and implant dentistry, including the ITI André Schroeder Research Prize, the International Association for Dental Research Young Investigator of the Year award in the field of implant dentistry, and the American Academy of Implant Dentistry Young Investigator grant award. He has completed postdoctoral research fellowships in Switzerland, Canada, China, Spain, and the United States.
Dr Richard J. Miron is currently Visiting Faculty in the Department of Periodontology at the University of Bern in Switzerland, where he completed his PhD studies. He has published over 150 peer-reviewed articles and lectures internationally on many topics relating to growth factors, bone biomaterials, and guided bone regeneration. Dr Miron has been awarded many top international prizes in regenerative dentistry and implant dentistry, including the ITI André Schroeder Research Prize, the International Association for Dental Research Young Investigator of the Year award in the field of implant dentistry, and the American Academy of Implant Dentistry Young Investigator grant award. He has completed postdoctoral research fellowships in Switzerland, Canada, China, Spain, and the United States. Dr Yufeng Zhang is the Luojiashan Distinguished Professor and chief physician at the Wuhan University Medical and Dental School in Wuhan, China. He completed a two-year peri-implant bone biology research fellowship at Queensland University of Technology in Brisbane, Australia, and in 2010 he completed an ITI scholar position at the University of Bern in Switzerland. His research is primarily engaged in the field of implanted biomaterials used for alveolar bone and periodontal regeneration. Dr Zhang was one of the first researchers to propose the concept of gene-activated tissue engineering scaffolds, developing a scaffold-gene integration system that has its own biologic activity in vivo due to the autocrine growth factor. He has since been responsible for the development of several biomaterials with numerous industrial partners.
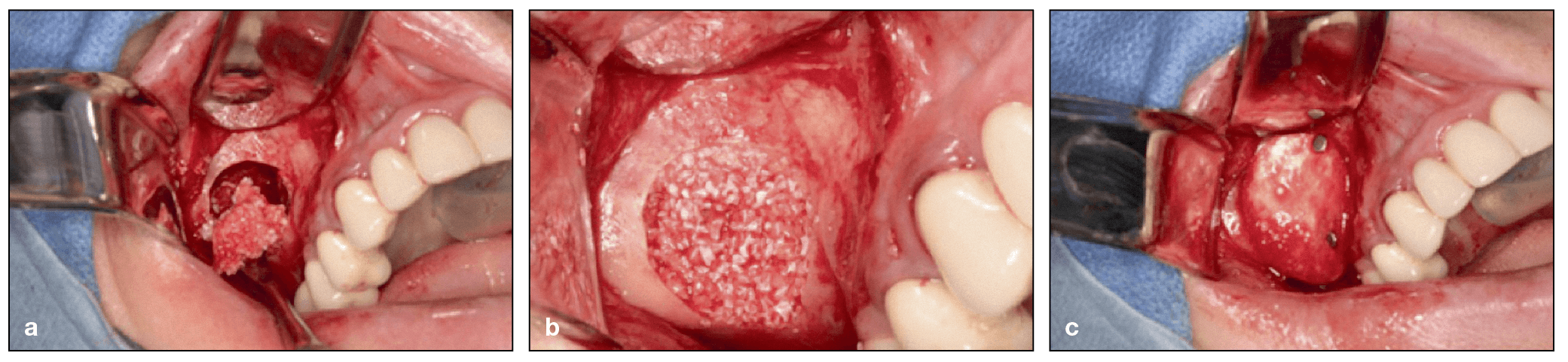
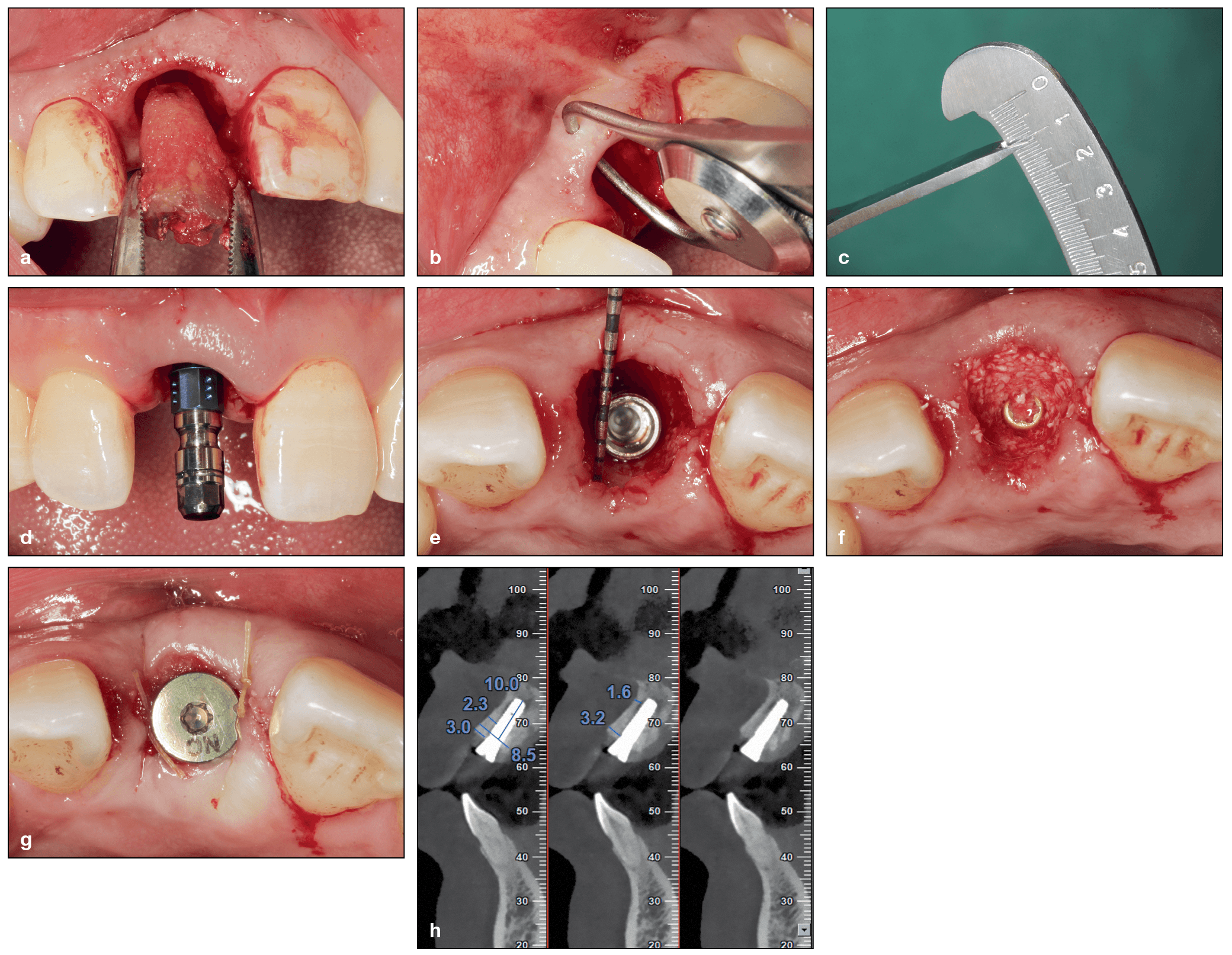
Dr Yufeng Zhang is the Luojiashan Distinguished Professor and chief physician at the Wuhan University Medical and Dental School in Wuhan, China. He completed a two-year peri-implant bone biology research fellowship at Queensland University of Technology in Brisbane, Australia, and in 2010 he completed an ITI scholar position at the University of Bern in Switzerland. His research is primarily engaged in the field of implanted biomaterials used for alveolar bone and periodontal regeneration. Dr Zhang was one of the first researchers to propose the concept of gene-activated tissue engineering scaffolds, developing a scaffold-gene integration system that has its own biologic activity in vivo due to the autocrine growth factor. He has since been responsible for the development of several biomaterials with numerous industrial partners. As research proceeds on treatment of the resorbed posterior maxilla, new techniques and innovations continue to be adopted to solve this clinical problem. While the previous edition of The Sinus Bone Graft provided detailed information on the types of grafting materials and procedures available at the time, this completely revised version looks to the future with new strategies for treatment, some of which avoid grafting altogether. Learn more in this Introduction to the book by Hilt Tatum Jr,
As research proceeds on treatment of the resorbed posterior maxilla, new techniques and innovations continue to be adopted to solve this clinical problem. While the previous edition of The Sinus Bone Graft provided detailed information on the types of grafting materials and procedures available at the time, this completely revised version looks to the future with new strategies for treatment, some of which avoid grafting altogether. Learn more in this Introduction to the book by Hilt Tatum Jr,