 Few names in modern oral and maxillofacial surgery are as respected as that of Daniel M. Laskin, DDS, MS. Throughout his career, Dr Laskin has made significant contributions to the specialty through his research, literature, and teaching and has also contributed immensely to the advancement of the specialty through his involvement in professional organizations. To commemorate the recent publication of the second edition of the Clinician’s Handbook of Oral and Maxillofacial Surgery, we offer this Author Spotlight in celebration of Dr Laskin’s incredible career and in gratitude for his contributions to our own body of publications.
Few names in modern oral and maxillofacial surgery are as respected as that of Daniel M. Laskin, DDS, MS. Throughout his career, Dr Laskin has made significant contributions to the specialty through his research, literature, and teaching and has also contributed immensely to the advancement of the specialty through his involvement in professional organizations. To commemorate the recent publication of the second edition of the Clinician’s Handbook of Oral and Maxillofacial Surgery, we offer this Author Spotlight in celebration of Dr Laskin’s incredible career and in gratitude for his contributions to our own body of publications.
A Legacy of Excellence
Temporomandibular Disorders: An Evidence-Based Approach to Diagnosis and Treatment, edited by Daniel M. Laskin, Charles S. Greene, and William L. Hylander (Quintessence, 2006)
Dr Laskin received his dental degree from the Indiana University School of Dentistry in 1947. He then completed a 1-year internship in oral surgery at the Jersey City Medical Center in Jersey City, New Jersey, in 1948 and his postgraduate studies in oral surgery at the University of Illinois at Chicago (UIC) College of Dentistry in Chicago, Illinois, in 1950. In 1951 he completed a master of science in oral pathology at UIC and a 1-year residency in oral surgery at the John H. Stroger Jr. Hospital of Cook County in Chicago, Illinois.
Dr Laskin remained at the UIC College of Dentistry for more than three decades, departing in 1983 as Professor Emeritus. During his tenure there, Dr Laskin taught both in the Department of Oral and Maxillofacial Surgery of the College of Dentistry, where he served as Head of Department from 1973 to 1983, and in the Department of Surgery of the College of Medicine, where he served as Director of the Postgraduate and Graduate Program for the Department of Oral and Maxillofacial Surgery from 1955 to 1983. He also served as Director of the UIC Temporomandibular Joint and Facial Pain Research Center from 1963 to 1983 and as Director of the Oral Surgery Residency Training Program at John H. Stroger Jr. Hospital of Cook County.
Decision Making in Oral and Maxillofacial Surgery, edited by Daniel M. Laskin and Omar A. Abubaker (Quintessence, 2007)
In 1984, Dr Laskin made the move from Chicago to Richmond, Virginia, to serve as Professor and Chairman of the Department of Oral and Maxillofacial Surgery at the Virginia Commonwealth University (VCU) School of Dentistry and of the Division of Oral and Maxillofacial Surgery of the Department of Surgery at the VCU School of Medicine. He directed the VCU Temporomandibular Joint and Facial Pain Research Center from 1984 to 2002. He achieved Chairman Emeritus status from the VCU School of Dentistry in 2002, where he remains involved and continues to lecture.
Treatment of TMDs: Bridging the Gap Between Advances in Research and Clinical Patient Management, edited by Charles S. Greene and Daniel M. Laskin (Quintessence, 2013)
“Dr Daniel Laskin is the quintessential oral and maxillofacial surgery educator,” says Eric Carlson, DMD, MD, EdM, coeditor of the Clinician’s Handbook of Oral and Maxillofacial Surgery, Second Edition. “He has devoted his entire career to education and has impacted every oral and maxillofacial surgeon over the past 50 years of our specialty’s existence. In short, Dan Laskin is synonymous with oral and maxillofacial surgery, and our entire specialty owes him a debt of gratitude. In paying homage to Dr Laskin, I simultaneously acknowledge all oral and maxillofacial surgery educators who are like him in some small way.”
Over the course of his career, Dr Laskin has also served the specialty through his involvement in various national and international professional organizations. He has served as President of the American Association of Oral and Maxillofacial Surgeons (1976–1977), the International Association of Oral and Maxillofacial Surgeons (1983–1986), and the National Academies of Practice (2002–2004). He is a fellow in Dental Surgery of the Royal College of Surgeons of England and the Royal College of Physicians and Surgeons of Glasgow (Hon). He is also a fellow of the American College of Dentists, the American Association for the Advancement of Sciences, the International College of Dentists, and the American Dental Society of Anesthesiology. The list of honors and awards he has received runs two pages long and includes the American Association of Oral and Maxillofacial Surgeons Research Recognition Award in 1978, the William J. Gies Oral Surgery Award in 1979, the American Dental Society of Anesthesiology Heidbrink Award in 1983, and the Donald B. Osbon Award for Outstanding Educator in 1991.
Oral and Maxillofacial Surgery Review: A Study Guide, edited by Din Lam and Daniel M. Laskin (Quintessence, 2015)
Dr Laskin’s research throughout his career has focused on the fields of connective tissue physiology and pathology, craniofacial growth, and the temporomandibular joint and its disorders. He has authored or coauthored more than 900 publications in OMFS and dental research and has won the William J. Gies Editorial Award 8 times with 10 Honorable Mentions. He is the author or coauthor of 18 books, including 6 with Quintessence Publishing.
The Book: Clinician’s Handbook of Oral and Maxillofacial Surgery, Second Edition

The Clinician’s Manual of Oral and Maxillofacial Surgery, edited by Paul H. Kwon and Daniel M. Laskin (Quintessence, 2001)
The Clinician’s Handbook of Oral and Maxillofacial Surgery was originally adapted from the Clinician’s Manual of Oral and Maxillofacial Surgery, which was edited by Dr Paul H. Kwon and Dr Laskin and saw three editions published between 1991 and 2001.
“The first edition of the Clinician’s Handbook of Oral and Maxillofacial Surgery,” Dr Laskin explains, “was designed to be portable in order to make the information immediately available. However, the amount of information necessary to include made it impossible to accomplish that goal. Therefore, the decision was made for the second edition to further increase the size so that more chapters, illustrations, and summary tables could be included, adding to the usefulness of the book. Condensing easy-to-access, pertinent information for the entire scope of the specialty is an impossible task for one person. However, selecting contributing authors with particular expertise in the various areas helped us achieve that goal and provide the information in a concise, organized manner.”
“As editors of this book, we endorsed individuality for all authors to format their chapters to be practically useful to our readership,” Dr Carlson adds. “We did not insist on a uniform presentation of the chapters, but rather gave authors permission to autonomously format their chapters to make high-yield information readily apparent to the readership in the best interests of proper patient care.”
The updates to both the format and the scope of this second edition contribute to the usefulness of the book as an important clinical resource by putting more of what the practicing oral and maxillofacial surgeon needs into one convenient reference source. It solves the issue of the time-consuming search for a current, reputable, scientifically proven solution for an immediate clinical problem. New chapters have been added on implantology, cleft lip and palate, maxillofacial reconstruction, oral squamous cell carcinoma, and cosmetic surgery.
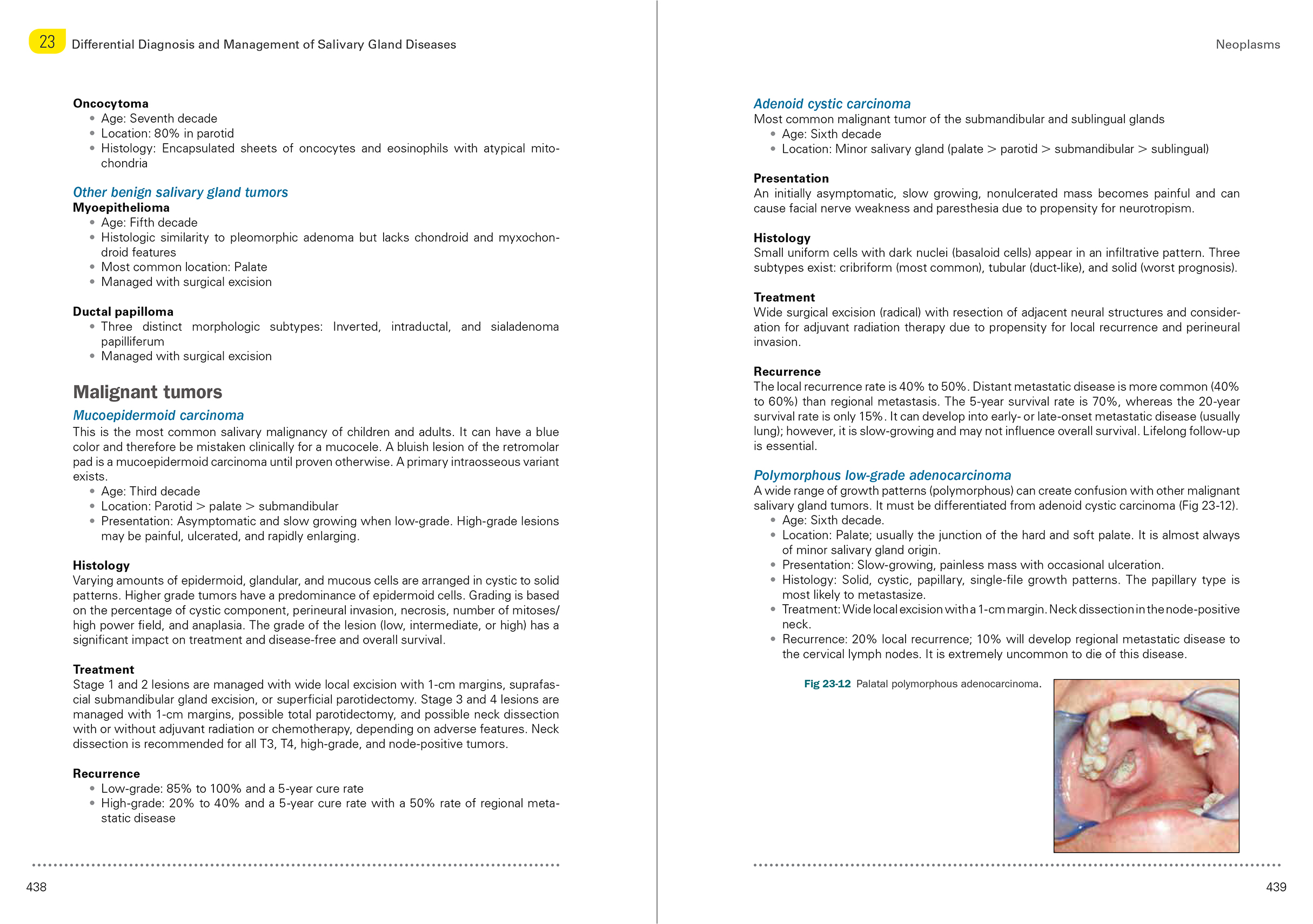
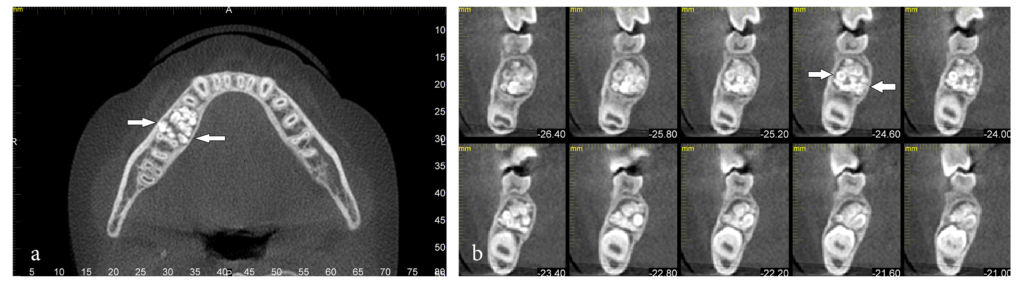
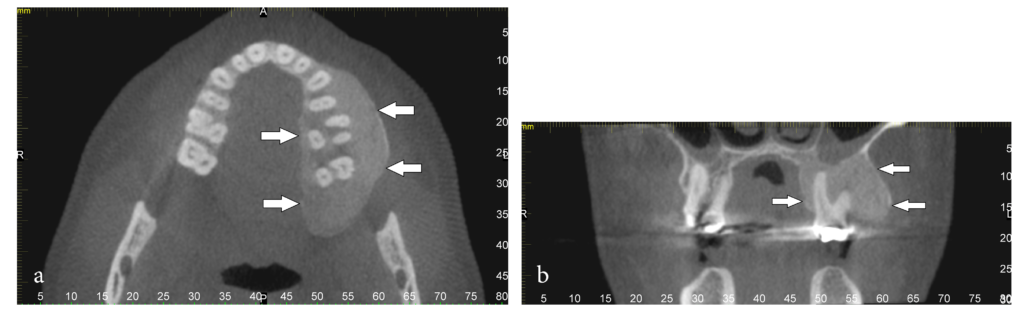
An example page spread from the expanded second edition of the Clinician’s Handbook of Oral and Maxillofacial Surgery.
“I have produced two types of books,” Dr Laskin says. “I have edited comprehensive textbooks on temporomandibular disorders that bring together experts to provide detailed information on one specific subject, and then there are those like this book that gathers and summarizes information from the entire specialty—pieces that would ordinarily be found in various different sources—into one site for quick reference. Although both types of books serve different purposes, in totality they provide the necessary information for practicing clinicians as well as residents to remain current in the specialty.”
The Clinician’s Handbook of Oral and Maxillofacial Surgery, Second Edition is not intended to replace the exhaustive textbook; instead, it synthesizes the information learned in postgraduate study and residency into a practical, clinically accessible format that clinicians can read cover to cover to review and familiarize themselves with the organization of information, then consult quickly for on-the-spot questions and answers as well as protocol validation.
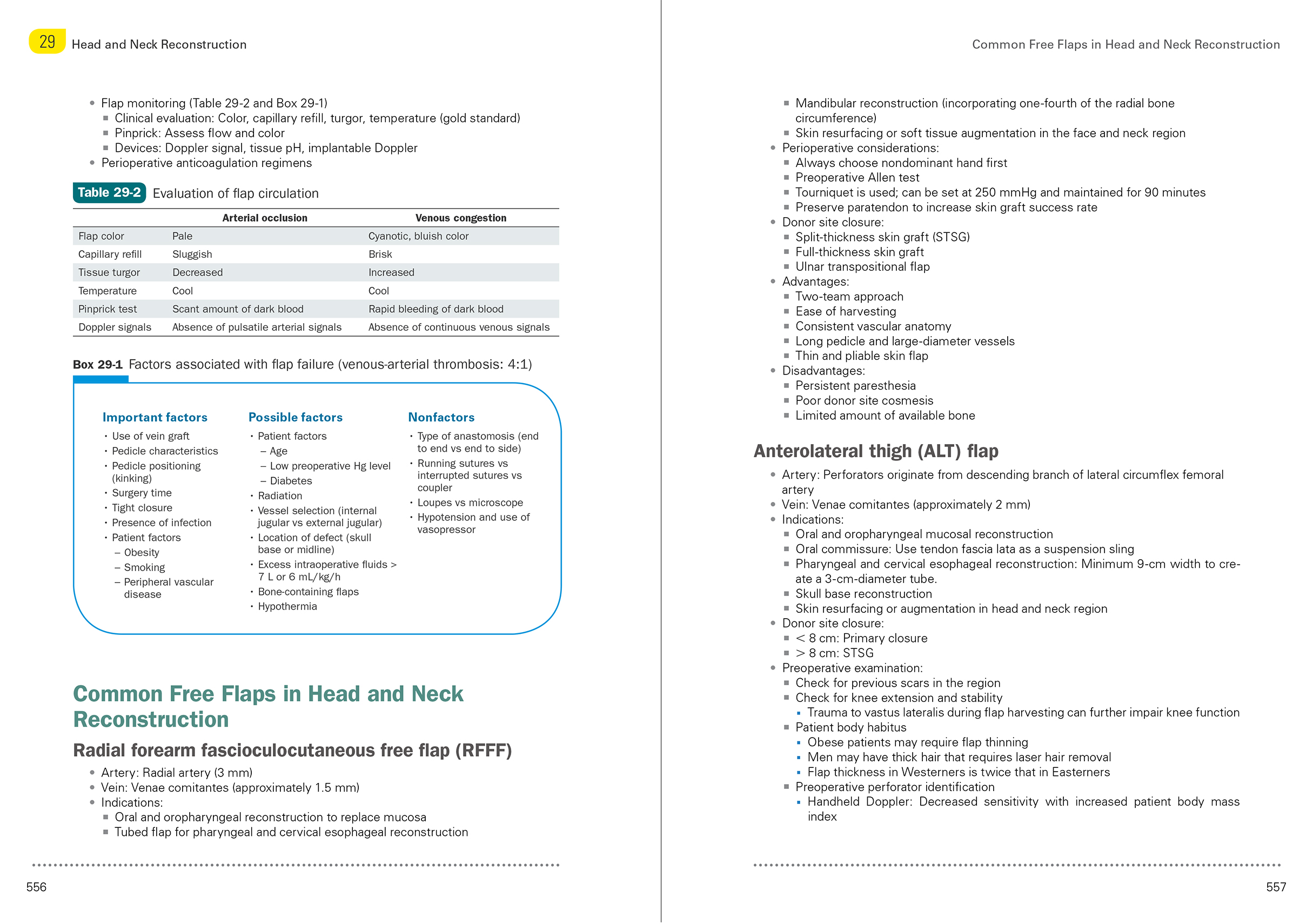
An example page spread from the expanded second edition of the Clinician’s Handbook of Oral and Maxillofacial Surgery.
“The popularity of this type of book,” Dr Laskin observes, “is indicated by the fact that this book ran for three editions in its original format and is now entering its second edition in the new format. For clinicians, this book still serves as a quick way to gain information in one place that ordinarily might be contained in various sources. For residents, it serves a similar purpose, as well as a good resource in preparation for the American Board of Oral and Maxillofacial Surgery.”
With the age of this book in both of its formats currently standing at just 27 years—young compared with many long-running textbooks—it is important to consider the future for a book with this level of impact and reputation, something Dr Laskin has certainly kept in mind while planning this second edition. In addition to expanding the format to increase the scope and impact of the book, he also brought in Dr Carlson as his coeditor.
“Because I am approaching the end of my career,” Dr Laskin says, “I made the decision to include a coeditor with outstanding academic and clinical credentials on this edition so that this publication will continue to be available in the future.”
“It is particularly meaningful to me,” Dr Carlson says, “that—at the age of 94—Dr Laskin continues to make outstanding contributions to our specialty’s literature. I feel honored to have served as Dr Laskin’s coeditor of this very important work. In many respects, peer-reviewed publications have supplanted textbooks in terms of their ability to provide current and meaningful evidence-based information for educational and patient-care purposes. However, textbooks and handbooks like this title go further than peer-reviewed publications can go by gathering a large body of current research, clinical results, and expert analysis into a comprehensive and cohesive reference source. Based on these realizations, it is always essential to plan the issue of a second edition of an important textbook. The information contained within the second edition is in keeping with providing current and meaningful information to trainees and practicing surgeons in our specialty. Furthermore, the incorporation of high-quality color images and illustrations enhances the educational value of the written information. I anticipate that the readership will peruse this textbook in preparation for challenging patient-care scenarios to ensure their adherence to current best practices.”
Reflections of Gratitude
As Dr Laskin reflects on his career, we reflect on the impact of his contributions to the field as well as our relationship with him as his publisher. It has been our pleasure to publish six books with Dr Laskin, and we have come to appreciate him as an editor with a well-developed vision for all of his publications, a reliable sense of attention to detail, and the clear communication skills necessary to coordinate a large group of contributors. In each project we have done with him, he has provided strong guidance and an incomparable source of knowledge and feedback while we have done our best to bring his visions to life on the page.
“Unlike with the conglomerate publishers,” Dr Laskin says, “working with Quintessence is like working with a family. You receive personal attention, you get to know the people with whom you work, and everyone’s goal is to produce an outstanding publication.”
Some people have a curriculum vitae so impressive that outstanding becomes the result the rest of us come to expect from that person because it has been achieved so many times before, and Dr Laskin is a true exemplar of this. It has been our pleasure to be his publisher, and we offer him our sincerest gratitude for the indelible effect he has had on the field of oral and maxillofacial surgery as well as on our world of dental publishing.
 Daniel M. Laskin, DDS, MS, has been a major contributor to the field of oral and maxillofacial surgery for more than 50 years. He received his dental degree from the Indiana University School of Dentistry in Indianapolis, Indiana, and his master of science in oral pathology from the University of Illinois at Chicago (UIC) in Chicago, Illinois. He completed his postgraduate studies in oral surgery at UIC and a 1-year residency at the John H. Stroger Jr. Hospital of Cook County in Chicago, Illinois. He served at the UIC College of Dentistry for more than 30 years, departing in 1983 as Professor Emeritus. In 1984, he left Chicago to serve as Professor and Chairman of the Department of Oral and Maxillofacial Surgery at the VCU School of Dentistry and of the Division of Oral and Maxillofacial Surgery of the Department of Surgery at the VCU School of Medicine. He directed the VCU Temporomandibular Joint and Facial Pain Research Center from 1984 to 2002. He achieved Chairman Emeritus status from the VCU School of Dentistry in 2002, where he remains involved and continues to lecture. He has served as President of the American Association of Oral and Maxillofacial Surgeons (1976–1977), the International Association of Oral and Maxillofacial Surgeons (1983–1986), and the National Academies of Practice (2002–2004). He is a fellow in Dental Surgery of the Royal College of Surgeons of England and the Royal College of Physicians and Surgeons of Glasgow (Hon). He is also a fellow of the American College of Dentists, the American Association for the Advancement of Sciences, the International College of Dentists, and the American Dental Society of Anesthesiology. He has served on the editorial board of more than 20 publications, contributed to more than 900 publications in OMFS and dental research, and has authored or co-authored 18 books. Throughout his career, Dr Laskin’s research has focused on connective tissue physiology and pathology, craniofacial growth, and the temporomandibular joint. His contributions to the field and his dedication to dental education have earned him a large number of honors and fellowships, and the impacts of his career will continue to benefit the field of oral and maxillofacial surgery for decades to come.
Daniel M. Laskin, DDS, MS, has been a major contributor to the field of oral and maxillofacial surgery for more than 50 years. He received his dental degree from the Indiana University School of Dentistry in Indianapolis, Indiana, and his master of science in oral pathology from the University of Illinois at Chicago (UIC) in Chicago, Illinois. He completed his postgraduate studies in oral surgery at UIC and a 1-year residency at the John H. Stroger Jr. Hospital of Cook County in Chicago, Illinois. He served at the UIC College of Dentistry for more than 30 years, departing in 1983 as Professor Emeritus. In 1984, he left Chicago to serve as Professor and Chairman of the Department of Oral and Maxillofacial Surgery at the VCU School of Dentistry and of the Division of Oral and Maxillofacial Surgery of the Department of Surgery at the VCU School of Medicine. He directed the VCU Temporomandibular Joint and Facial Pain Research Center from 1984 to 2002. He achieved Chairman Emeritus status from the VCU School of Dentistry in 2002, where he remains involved and continues to lecture. He has served as President of the American Association of Oral and Maxillofacial Surgeons (1976–1977), the International Association of Oral and Maxillofacial Surgeons (1983–1986), and the National Academies of Practice (2002–2004). He is a fellow in Dental Surgery of the Royal College of Surgeons of England and the Royal College of Physicians and Surgeons of Glasgow (Hon). He is also a fellow of the American College of Dentists, the American Association for the Advancement of Sciences, the International College of Dentists, and the American Dental Society of Anesthesiology. He has served on the editorial board of more than 20 publications, contributed to more than 900 publications in OMFS and dental research, and has authored or co-authored 18 books. Throughout his career, Dr Laskin’s research has focused on connective tissue physiology and pathology, craniofacial growth, and the temporomandibular joint. His contributions to the field and his dedication to dental education have earned him a large number of honors and fellowships, and the impacts of his career will continue to benefit the field of oral and maxillofacial surgery for decades to come.
 Eric R. Carlson, DMD, MD, EdM, is Professor and Kelly L. Krahwinkel Chairman of the Department of Oral and Maxillofacial Surgery at the University of Tennessee, where he also serves as Director of the Oral and Maxillofacial Surgery Residency Program and the Oral/Head and Neck Oncologic Surgery Fellowship Program. He received his dental degree from the University of Pennsylvania School of Dental Medicine, his medical degree from the University of Miami Leonard M. Miller School of Medicine, and his master of education degree from the Harvard University Graduate School of Education. Dr Carlson is a fellow of the American College of Surgeons and has previously served as Chair of the American Association of Oral and Maxillofacial Surgeons Special Committee on Oral and Maxillofacial Surgery Parameters of Care, as the Oral and Maxillofacial Surgery Commissioner for the Commission on Dental Accreditation (CODA), and as Chair of the CODA Oral and Maxillofacial Surgery Residency Review Committee. He has also served as the Surgical Oncology and Reconstruction Section Editor for the Journal of Oral and Maxillofacial Surgery. Dr Carlson’s clinical expertise is in oral/head and neck tumor surgery, and his research focuses on the molecular aspects of cancer diagnosis and treatment.
Eric R. Carlson, DMD, MD, EdM, is Professor and Kelly L. Krahwinkel Chairman of the Department of Oral and Maxillofacial Surgery at the University of Tennessee, where he also serves as Director of the Oral and Maxillofacial Surgery Residency Program and the Oral/Head and Neck Oncologic Surgery Fellowship Program. He received his dental degree from the University of Pennsylvania School of Dental Medicine, his medical degree from the University of Miami Leonard M. Miller School of Medicine, and his master of education degree from the Harvard University Graduate School of Education. Dr Carlson is a fellow of the American College of Surgeons and has previously served as Chair of the American Association of Oral and Maxillofacial Surgeons Special Committee on Oral and Maxillofacial Surgery Parameters of Care, as the Oral and Maxillofacial Surgery Commissioner for the Commission on Dental Accreditation (CODA), and as Chair of the CODA Oral and Maxillofacial Surgery Residency Review Committee. He has also served as the Surgical Oncology and Reconstruction Section Editor for the Journal of Oral and Maxillofacial Surgery. Dr Carlson’s clinical expertise is in oral/head and neck tumor surgery, and his research focuses on the molecular aspects of cancer diagnosis and treatment.
 Clinician’s Handbook of Oral and Maxillofacial Surgery, Second Edition
Clinician’s Handbook of Oral and Maxillofacial Surgery, Second Edition
Edited by Daniel M. Laskin and Eric R. Carlson
There are frequent situations in which oral and maxillofacial surgeons find themselves in need of an immediate answer to a clinical problem. However, this can involve a time-consuming search for the appropriate reference source. This book continues the format of the previous edition by providing a single place to quickly find information on a diverse range of clinical topics, including dentoalveolar surgery, maxillofacial trauma, craniofacial anomalies, and oral pathology. All of the previous chapters have been updated, and new chapters on implantology, cleft lip and palate, maxillofacial reconstruction, oral squamous cell carcinoma, and cosmetic surgery have been added. Moreover, increasing the size of the book has allowed for the inclusion of many summary charts, tables, clinical photographs, and radiographs, which was not possible in the previous version. As a result, this new edition provides expanded information in an improved format.
Although this book is designed as a quick reference source, familiarizing oneself with its content in advance will both add to the reader’s general knowledge base and improve the ability to find information quickly in urgent situations. Residents in oral and maxillofacial surgery should find its content particularly useful during their clinical training, and the concise organization of the material should also be helpful to them in retaining information when subsequently preparing for the American Board of Oral and Maxillofacial Surgery.
624 pp (softcover); 374 illus; ©2019; ISBN 978-0-86715-730-7 (B7307); $168










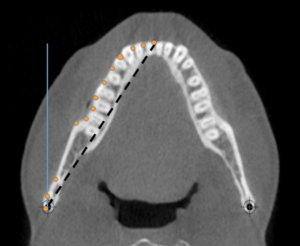
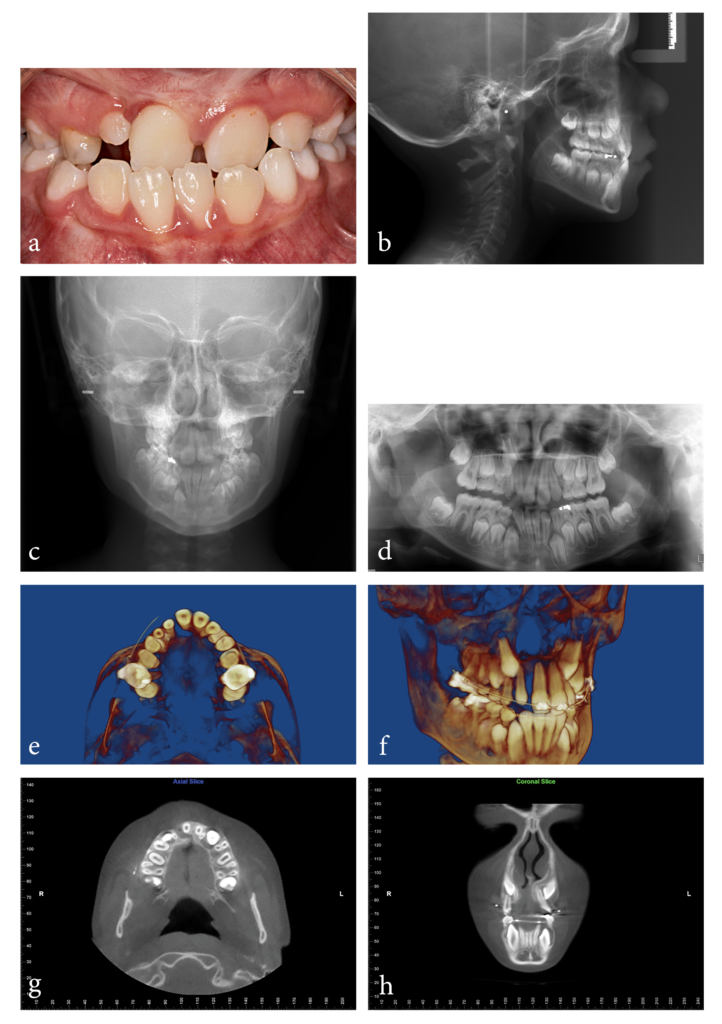
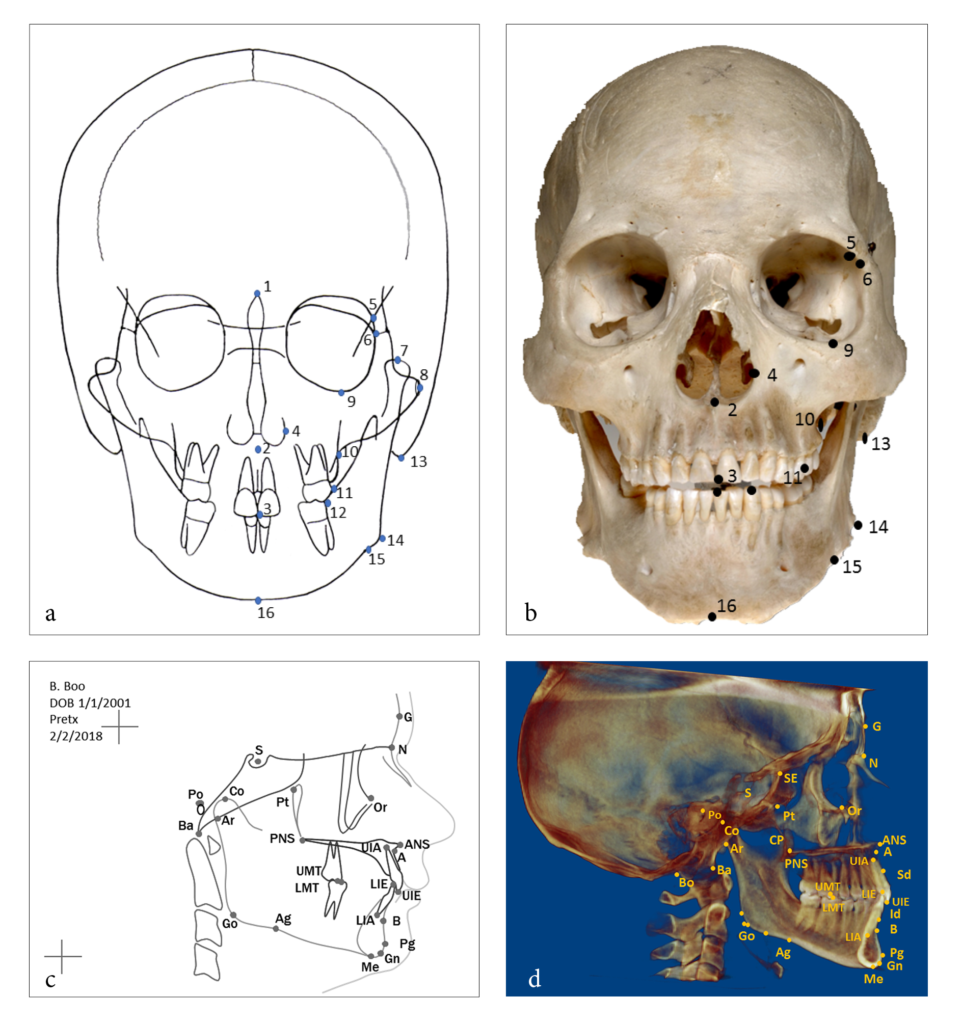
 Katherine Kula, MS, DMD, MS, retired as Jarabak Endowed Professor and Chairperson for the Department of Orthodontics and Oral Facial Genetics at the Indiana University School of Dentistry in Indianapolis, Indiana. A board-certified orthodontist, Dr Kula taught and practiced for more than 40 years. She has authored more than 100 papers and 18 chapters, edited 4 books and monographs, and is the recipient of several national research awards and grants. In addition to her activities in professional societies, Dr Kula organized the first meeting involving the American Dental Association (ADA) and the US Food and Drug Administration regarding the approval of dental therapeutics and devices, and her research is cited in the ADA’s stance concerning the effect of acidulated phosphate fluorides on dental materials. Her research interests currently include three-dimensional imaging, technology, music, growth and development of the craniofacial complex, and forensic facial reconstruction.
Katherine Kula, MS, DMD, MS, retired as Jarabak Endowed Professor and Chairperson for the Department of Orthodontics and Oral Facial Genetics at the Indiana University School of Dentistry in Indianapolis, Indiana. A board-certified orthodontist, Dr Kula taught and practiced for more than 40 years. She has authored more than 100 papers and 18 chapters, edited 4 books and monographs, and is the recipient of several national research awards and grants. In addition to her activities in professional societies, Dr Kula organized the first meeting involving the American Dental Association (ADA) and the US Food and Drug Administration regarding the approval of dental therapeutics and devices, and her research is cited in the ADA’s stance concerning the effect of acidulated phosphate fluorides on dental materials. Her research interests currently include three-dimensional imaging, technology, music, growth and development of the craniofacial complex, and forensic facial reconstruction. Ahmed Ghoneima, BDS, PhD, MSD, is Associate Professor of Orthodontics and Graduate Program Director of the College of Dental Medicine at Mohammed Bin Rashid University of Medicine and Health Sciences in Dubai, United Arab Emirates. He received his dental degree and master of science from Al-Azhar University in Cairo, Egypt, and his PhD from the Department of Orthodontics and Oral Facial Genetics at the Indiana University School of Dentistry in Indianapolis, Indiana, where he became a full-time faculty member. His research program focuses on airway analysis, applications of three-dimensional imaging in orthodontics, haptic technology, and the use of virtual reality in dental education. Dr Ghoneima is the recipient of numerous prestigious awards, including the Michael Matlof Memorial Teaching Fellowship Award and the Orhan C. Tuncay Teaching Fellowship Award, both from the American Association of Orthodontists Foundation, as well as the Academy for Academic Leadership Award. He has previously chaired the Indiana Section of the American Association for Dental Research and currently holds the position of Chair Elect for the American Dental Education Association section on orthodontics. He also serves as a reviewer for several peer-reviewed orthodontic journals.
Ahmed Ghoneima, BDS, PhD, MSD, is Associate Professor of Orthodontics and Graduate Program Director of the College of Dental Medicine at Mohammed Bin Rashid University of Medicine and Health Sciences in Dubai, United Arab Emirates. He received his dental degree and master of science from Al-Azhar University in Cairo, Egypt, and his PhD from the Department of Orthodontics and Oral Facial Genetics at the Indiana University School of Dentistry in Indianapolis, Indiana, where he became a full-time faculty member. His research program focuses on airway analysis, applications of three-dimensional imaging in orthodontics, haptic technology, and the use of virtual reality in dental education. Dr Ghoneima is the recipient of numerous prestigious awards, including the Michael Matlof Memorial Teaching Fellowship Award and the Orhan C. Tuncay Teaching Fellowship Award, both from the American Association of Orthodontists Foundation, as well as the Academy for Academic Leadership Award. He has previously chaired the Indiana Section of the American Association for Dental Research and currently holds the position of Chair Elect for the American Dental Education Association section on orthodontics. He also serves as a reviewer for several peer-reviewed orthodontic journals.








 Douglas Deporter, DDS, Dip Perio, PhD, has been a full-time member of the Faculty of Dentistry at the University of Toronto since 1976. He has been involved in clinical research in implant dentistry for over 30 years and has published extensively on short and ultra-short implants, particularly those with sintered porous-surfaced (SPS) topography. He was coinventor of the original SPS implant (Endopore), the patent for which was assigned to the University of Toronto. Dr Deporter has given more than 140 invited international presentations. He also maintains a part-time private practice limited to periodontics and implant dentistry in Toronto, Ontario.
Douglas Deporter, DDS, Dip Perio, PhD, has been a full-time member of the Faculty of Dentistry at the University of Toronto since 1976. He has been involved in clinical research in implant dentistry for over 30 years and has published extensively on short and ultra-short implants, particularly those with sintered porous-surfaced (SPS) topography. He was coinventor of the original SPS implant (Endopore), the patent for which was assigned to the University of Toronto. Dr Deporter has given more than 140 invited international presentations. He also maintains a part-time private practice limited to periodontics and implant dentistry in Toronto, Ontario.