When clear aligners were first released to the market in 1999, most clinicians understood them to be limited to the orthodontic treatment of Class I cases with minor crowding. While they presented as an esthetic treatment option for these minor correction cases, they did not claim significant territory overall from traditional fixed appliances due to their perceived treatment limitations. However, recent advances in digital technology in dentistry have resulted in explosive improvements in clear aligner technology, and these developments have brought the technology in line with the capabilities of fixed appliances. Clear Aligner Technique, a new clinical orthodontic textbook by Sandra Tai, BDS, MS, examines clear aligner treatment from this new perspective—that clear aligner technology is a comprehensive treatment modality that can both satisfy current clinical expectations and propel the field to new heights of success.

Modern Orthodontics and the Rise of Clear Aligner Technology
Clear aligner technique requires a paradigm shift in the thought process from being a reactive orthodontist to being a proactive orthodontist.
“There is a distinct difference between evolutionary change and revolutionary change,” Dr Sandra Tai explains. “Evolutionary change comprises incremental changes that take place gradually over time. The evolution of fixed appliances represents variations and incremental improvements on a bracket and wire system that has taken place over the last 100 years. Revolutionary change, in contrast, is transformational change. Revolutionary change is profound, dramatic, and disruptive. Revolutionary change challenges conventional thinking and requires a radical paradigm shift in our mindset. Clear aligner technology represents a revolutionary, transformational change in orthodontics that challenges the conventional thinking of how orthodontists move teeth.
“However,” she continues, “the advent of clear aligner technology does not mean that 150 years of orthodontic principles are no longer valid. The time-tested principles and concepts of bone biology, biomechanics, anchorage, and occlusion still apply. The challenge in this 21st century of digital technology is that the clinician must now learn to apply those principles of orthodontics to the field of clear aligner technique.”
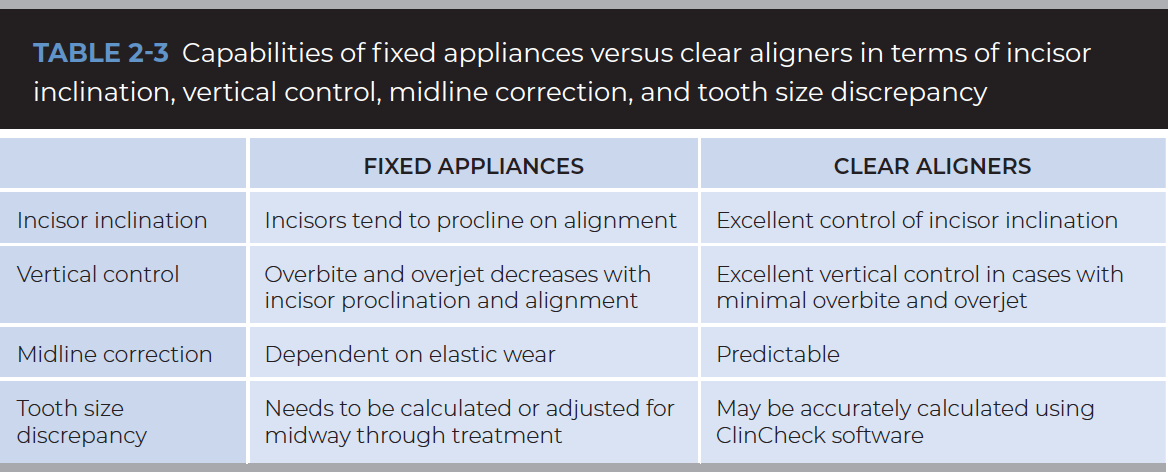
There are also significant differences between techniques for fixed appliances and aligners that clinicians must understand. “One fundamental difference,” Dr Tai explains, “is between the way a bracket and wire system moves teeth and the way clear aligners move teeth. Fixed appliances pull on teeth while clear aligners push teeth. In the illustration below, you can see that when an archwire is engaged onto a lingually erupted tooth, the elasticity in the archwire causes the archwire to return to its original arch form. As the archwire returns to its original shape, it pulls on the lingually erupted tooth to move it into the arch. The force applied to the tooth is dependent on the flexibility of the archwire and the amount of deflection it undergoes to engage the tooth. In contrast, clear aligners move teeth by exerting a push force. When an aligner is inserted over teeth, there are minor differences between the positions of the teeth intraorally and the positions of the teeth in the aligner. The aligner deforms over the teeth, and the elasticity in the aligner material pushes the teeth into position. Optimized attachments provide an active, flat surface that the aligner may push against to effect tooth movements such as extrusion or rotation.

As the archwire reverts to its original form, it pulls the lingually erupted tooth into the dental arch.
Clear aligner treatment is a technique, not a product.
Realizing the Full Potential of Clear Aligner Technique
Another area of clear aligner technique where clinicians must revise their knowledge is in their clinical expectations for these appliances.
“Many clinicians and patients think that aligners can only be used for slight corrections versus a complete treatment,” Dr Tai says, “and I would say that this impression may have been correct for the aligners available 15 years ago. However, the technology, material, and software algorithms have evolved significantly since then. Today, clear aligners are the orthodontic appliance of choice for a wide range of occlusions.”
Dr Tai’s personal revelation regarding clear aligner technology’s treatment capabilities came when she treated a touring gospel singer. The catch? The patient lived in New Zealand, and Dr Tai’s practice is in Vancouver, Canada. “Her band toured in North America 4 times a year, and she committed to seeing me every 3 months,” Dr Tai recalls. “Our only option was aligner treatment. The case treated out well with no complications, and it was then that I realized no patient is ‘too far’ and that even challenging cases can be successfully treated with clear aligners. Today, I have patients who fly in to see me from all over the world for clear aligner treatment.
“It is important to understand that clear aligner treatment is a technique, not a product,” Dr Tai continues. “The common misconception is that clear aligners are a ‘compromise’ orthodontic treatment, either prescribed for only minor correction or when a patient’s main concern is esthetics. However, the clear aligner system of today is a comprehensive orthodontic appliance, capable of treating a wide range of malocclusions when in the hands of an experienced clinician.”
The following case—one of many shown in Dr Tai’s book—serves as a striking example of the degree of clinical success that can be achieved with clear aligner technique.

(a to j) Pretreatment records. The patient presents with a Class II malocclusion with facial asymmetry and a canted maxillary occlusal plane.

(k to m) Superimpositions in the software plan demonstrating the amount of anterior intrusion and incisor retraction. (n) The Tooth Movement Assessment shows that the anterior intrusion in the maxillary left quadrant is considered a moderately difficult tooth movement.

(o to s) Progress photographs showing the aligners in place with intraoral elastics running from the buccal TAD to the lingual TAD as well as interarch Class II elastics worn for anchorage.

(t to x) Progress photographs taken at the end of the first series of aligners. The extraction spaces have closed, and both dental arches are well aligned. Another set of aligners is required to detail root inclinations and further correct the buccal relationship on the right side to Class I canine and Class II molar. (y and z) Comparison of pretreatment and progress facial photographs showing the improvement in smile esthetics.
The Danger of DIY Aligner Products
To move teeth without first ascertaining overall oral health, caries risk, periodontal status, and taking radiographs would amount to malpractice in the place where I practice.
“I think patients need to understand that DIY orthodontic companies are not just offering cosmetic services to make you look more beautiful,” Dr Tai says. “It is not the appliance that treats the patient. It is the orthodontist’s clinical expertise in making a proper diagnosis, treatment planning, and executing the treatment clinically that treats the patient. Moving teeth and changing the bite should only be done within the context of proper diagnosis and an understanding of the occlusion. To move teeth without first ascertaining overall oral health, caries risk, periodontal status, and taking radiographs would amount to malpractice in the place where I practice.”
Many general dentists are also now providing treatment with clear aligners, and while their level of expertise and practice model can in no way be compared to mail-order aligner companies, they still need to understand their limitations. “General practitioners may receive some orthodontic training in dental school or attend continuing education courses to recognize, diagnose, and treat simple malocclusions,” Dr Tai explains. “However, just as a family physician may treat high blood pressure but refer a patient who develops coronary artery disease to a cardiologist, general practitioners must be able to recognize and refer complex malocclusions, particularly in patients with underlying skeletal problems, to an orthodontist for treatment.”
An International Perspective
 Part of what makes Dr Tai’s perspective unique is her international experience as a student, as an educator, and as a clinician. Born in Aldershot, England, she studied dentistry at the University of Malaya in Kuala Lumpur, Malaysia, and obtained her certificate in orthodontics at the University of Minnesota in Minneapolis. Since opening her practice in Vancouver, British Columbia, she has continued to lecture internationally, which has resulted in a clinical textbook applicable to dental practices across the globe.
Part of what makes Dr Tai’s perspective unique is her international experience as a student, as an educator, and as a clinician. Born in Aldershot, England, she studied dentistry at the University of Malaya in Kuala Lumpur, Malaysia, and obtained her certificate in orthodontics at the University of Minnesota in Minneapolis. Since opening her practice in Vancouver, British Columbia, she has continued to lecture internationally, which has resulted in a clinical textbook applicable to dental practices across the globe.
“Through my education, travel, and clinical experience, I have learned that there are different orthodontic philosophies all over the world,” Dr Tai explains. “Malocclusions vary by ethnicity, and some populations have more complex malocclusions. For example, a high proportion of Asian malocclusions in China and Japan are treated with premolar extractions. In clear aligner treatment, the software programs that determine the tooth movements are customizable to accommodate these different approaches to orthodontic treatment. In our example of premolar extraction, these cases are often programmed for maximum anchorage. Extraction sites may also be closed in a variety of ways, such as with moderate anchorage considerations. In Japan, orthodontists use a technique called the staggered staging technique, where the canine is moved for 10 stages then stops, then the incisors are retracted for 10 stages then stop, then the canine is moved another 10 stages, and the sequence is repeated until the extraction spaces are closed.”

The staggered staging technique as shown in the clear aligner treatment planning software. (Courtesy of Dr Hiroshi Samoto, Tokyo, Japan.)
Just as it would be hard to prescribe one orthodontic treatment philosophy to every distinct population group in the world, it can be hard to write a clinical orthodontic textbook applicable to many different markets. Through the combination of her professional experience and the fact that clear aligners are available internationally with customizable treatment software designed to individualize treatment based on the patient, Dr Tai’s book accomplishes just that.
“I started lecturing globally in 2011,” she says. “As a result of my travels and interacting with professional colleagues all over the world, I have become more broad-minded and accepting of various orthodontic approaches to treatment. Everywhere I went, dentists and orthodontists expressed interest in learning more about clear aligners and wanted to know what textbook I could recommend. There were no good resources available, so I decided to write my own! It took 6 years to develop the teaching material that forms the foundation and contents of the textbook, which incorporates everything I’ve learned through my practice and my professional travels.”
The Future of Orthodontics
Clear aligner technology has gained significant momentum in recent years, and Dr Tai says this technology shows no signs of slowing down.
“I see clear aligner technology as the future of orthodontics,” she explains. “Just as we now look back on the full-banded appliances of Edward Angle’s day and realize how far orthodontics has evolved and developed since then, one day we will look back at bracket and wire systems in the same way. Clear aligners are part of the larger picture of the digital age and how this era has affected every part of our lives from computers to mobile phones to advances in medicine and dentistry. Dentistry itself now has CBCT for diagnosis and treatment planning, CAD/CAM–milled crowns, 3D-printed models, and digital impressions—a digitally produced orthodontic appliance such as clear aligners is part of this revolution in the technological age. The power of digital treatment planning and the ability to design occlusions with customized tip, torque, and arch forms enables us to serve our patients better and deliver superior treatment outcomes. As clear aligner technique continues to evolve, there is no doubt that one day soon we will be able to treat all malocclusions with clear aligners, and bracket and wire systems will become part of our history.”
As to where her book Clear Aligner Technique fits into this timeline, Dr Tai sees it as an integral piece in bridging the foundation of orthodontic knowledge developed and refined previously with these new advances in digital technology and clear aligner technique.
“I think this book will revolutionize the way dentists and orthodontists think about the future of orthodontics and clear aligners,” she explains. “It establishes clear aligners as a valid orthodontic technique that is capable of treating a wide range of malocclusions. Over and above that, it also demonstrates how clear aligners—when in the hands of a well-trained clinician—are capable of delivering finished results to the same standard of excellence as traditional bracket and wire systems. As both a clinician and educator in this field, my hope is that dental schools will start incorporating clear aligner technique into their curriculum for training orthodontists and dentists. This textbook will be a great resource for educators everywhere. As we move forward, it is also imperative that we take the field of clear aligners seriously and devote the time to do the scientific research that is necessary so that we continue to practice clinically sound, evidence-based orthodontics.”
Dr Tai closes with a quote from her book: “‘The future lies in continuing to innovate with passion to transform the future of our profession.’ At the heart of it all, we are changing smiles and changing lives.”

 Sandra Tai, BDS, MS, has been an Invisalign certified orthodontist since 2000 and is currently an Invisalign Top 1%/Diamond Provider who has treated over 1,500 cases with Invisalign. As an editorial board member for the Journal of Aligner Orthodontics and a member of Align Tech Faculty in North America, she is involved in several clinical research projects and FDA clinical research trials with clear aligners. Dr Tai is currently a clinical assistant professor in Orthodontics as well as the coordinator for the Invisalign program at the University of British Columbia in Vancouver. She also maintains a busy international lecture schedule, speaking to orthodontists all over the world about clear aligners and their potential. Dr Tai is a Fellow of the College of Dental Surgeons of British Columbia and a Fellow of the Royal College of Dentists, Canada, as well as a member of several professional organizations. She is also the founding member and past president of the Orthodontic Ties Seminars Study Club in Vancouver and the Vancouver Invisalign Study Club, where she mentors and trains dentists in the Invisalign system. She received her graduate training in Orthodontics at the University of Minnesota.
Sandra Tai, BDS, MS, has been an Invisalign certified orthodontist since 2000 and is currently an Invisalign Top 1%/Diamond Provider who has treated over 1,500 cases with Invisalign. As an editorial board member for the Journal of Aligner Orthodontics and a member of Align Tech Faculty in North America, she is involved in several clinical research projects and FDA clinical research trials with clear aligners. Dr Tai is currently a clinical assistant professor in Orthodontics as well as the coordinator for the Invisalign program at the University of British Columbia in Vancouver. She also maintains a busy international lecture schedule, speaking to orthodontists all over the world about clear aligners and their potential. Dr Tai is a Fellow of the College of Dental Surgeons of British Columbia and a Fellow of the Royal College of Dentists, Canada, as well as a member of several professional organizations. She is also the founding member and past president of the Orthodontic Ties Seminars Study Club in Vancouver and the Vancouver Invisalign Study Club, where she mentors and trains dentists in the Invisalign system. She received her graduate training in Orthodontics at the University of Minnesota.
Sandra Tai
Clear aligners are the future of orthodontics, but digital orthodontics evolves so rapidly that it is hard to keep pace. This book approaches clear aligner treatment from a diagnosis and treatment-planning perspective, discussing time-tested orthodontic principles like biomechanics and anchorage and demonstrating how to apply them to orthodontic cases using these appliances. Each chapter explains how to use clear aligners to treat a given malocclusion and teaches clinicians how to program a suitable treatment plan using available software, how to design the digital tooth movements to match the treatment goals, and finally how execute the treatment clinically and finish the case well. This clinical handbook will prepare orthodontists and dental students to exceed patient expectations with the most esthetic orthodontic appliance currently available.
320 pp; 1,344 illus; ©2018; ISBN 978-0-86715-777-2 (B7772); US $218












 Reny de Leeuw, DDS, PhD, MPH, is Professor and Associate Dean for Academic Affairs of the Department of Orofacial Pain of the University of Kentucky College of Dentistry. She received both her DDS and PhD from RijksUniversiteit Groningen, The Netherlands, before completing an MPH and a residency in orofacial pain at the University of Kentucky. Her research interests include orofacial pain, temporomandibular disorders, posttraumatic stress disorder, and functional brain imaging. She is a fellow of the American Academy of Orofacial Pain and a diplomate of the American Board of Orofacial Pain, as well as editor of the fourth, fifth, and sixth editions of
Reny de Leeuw, DDS, PhD, MPH, is Professor and Associate Dean for Academic Affairs of the Department of Orofacial Pain of the University of Kentucky College of Dentistry. She received both her DDS and PhD from RijksUniversiteit Groningen, The Netherlands, before completing an MPH and a residency in orofacial pain at the University of Kentucky. Her research interests include orofacial pain, temporomandibular disorders, posttraumatic stress disorder, and functional brain imaging. She is a fellow of the American Academy of Orofacial Pain and a diplomate of the American Board of Orofacial Pain, as well as editor of the fourth, fifth, and sixth editions of  Gary D. Klasser, DMD, is Professor in the Division of Diagnostic Sciences at the Louisiana State University School of Dentistry in New Orleans. He obtained his dental degree from the University of Manitoba, Canada, in 1980. He then practiced general dentistry for the next 22 years before returning to graduate studies. In 2004, he received his certificate in orofacial pain from the University of Kentucky College of Dentistry. In 2005, he completed a fellowship in oral medicine/oral oncology at the University of Illinois at Chicago (UIC) College of Dentistry, where he served as Assistant Professor and Director of the oral medicine/orofacial pain clinic until 2011. Dr Klasser has published in a number of peer-reviewed journals, contributed chapters to various textbooks, and served as an editorial reviewer for a number journals. He is Council Chair for the American Academy of Orofacial Pain and coeditor of
Gary D. Klasser, DMD, is Professor in the Division of Diagnostic Sciences at the Louisiana State University School of Dentistry in New Orleans. He obtained his dental degree from the University of Manitoba, Canada, in 1980. He then practiced general dentistry for the next 22 years before returning to graduate studies. In 2004, he received his certificate in orofacial pain from the University of Kentucky College of Dentistry. In 2005, he completed a fellowship in oral medicine/oral oncology at the University of Illinois at Chicago (UIC) College of Dentistry, where he served as Assistant Professor and Director of the oral medicine/orofacial pain clinic until 2011. Dr Klasser has published in a number of peer-reviewed journals, contributed chapters to various textbooks, and served as an editorial reviewer for a number journals. He is Council Chair for the American Academy of Orofacial Pain and coeditor of  Ghabi Kaspo, DDS, has been practicing dentistry, primarily in the field of orofacial pain management, for the past 17 years. He received his dental degree and diploma in orthodontics from Damascus University in Syria and a second DDS from the University of Detroit Mercy in Michigan. He completed his certificate in orofacial pain management at the University of Medicine and Dentistry of New Jersey in Newark. He is a diplomate of the American Board of Orofacial Pain and of the American Board of Dental Sleep Medicine and is current President of the American Academy of Orofacial Pain. He has published numerous articles on topics such as temporomandibular imaging, fibromyalgia and sleep disorders in TMD patients, and headache. He maintains a private practice limited to orofacial pain management with locations in both Troy and Bingham Farms, Michigan.
Ghabi Kaspo, DDS, has been practicing dentistry, primarily in the field of orofacial pain management, for the past 17 years. He received his dental degree and diploma in orthodontics from Damascus University in Syria and a second DDS from the University of Detroit Mercy in Michigan. He completed his certificate in orofacial pain management at the University of Medicine and Dentistry of New Jersey in Newark. He is a diplomate of the American Board of Orofacial Pain and of the American Board of Dental Sleep Medicine and is current President of the American Academy of Orofacial Pain. He has published numerous articles on topics such as temporomandibular imaging, fibromyalgia and sleep disorders in TMD patients, and headache. He maintains a private practice limited to orofacial pain management with locations in both Troy and Bingham Farms, Michigan. After 20 years of exemplary leadership, Barry J. Sessle, BDS, MDS, BSc, PhD, DSc(hc), FRSC, will be stepping down from his position as Editor-in-Chief of the
After 20 years of exemplary leadership, Barry J. Sessle, BDS, MDS, BSc, PhD, DSc(hc), FRSC, will be stepping down from his position as Editor-in-Chief of the  certain that Dr Benoliel will uphold the journal’s reputation for excellence, and we look forward to seeing where his leadership takes the journal. Dr Benoliel is currently director at the Center for Orofacial Pain and Temporomandibular Disorders at the Rutgers School of Dental Medicine, where he also serves as associate dean for research. He completed his dental training with honors and distinction at the University of London. Following 2 years of training in oral and maxillofacial surgery, Dr Benoliel became part of the dental faculty at the Hebrew University Hadassah Medical School in Jerusalem. There, he completed a concentration in orofacial pain under the mentorship of Dr Yair Sharav and served as chair of the Department of Medicine from 2003 to 2010 before joining the dental school at Rutgers in 2013. Dr Benoliel has published extensively on the subject of orofacial pain, including over 120 articles, book chapters, and case reports. He is also co-editor of the award-winning textbook
certain that Dr Benoliel will uphold the journal’s reputation for excellence, and we look forward to seeing where his leadership takes the journal. Dr Benoliel is currently director at the Center for Orofacial Pain and Temporomandibular Disorders at the Rutgers School of Dental Medicine, where he also serves as associate dean for research. He completed his dental training with honors and distinction at the University of London. Following 2 years of training in oral and maxillofacial surgery, Dr Benoliel became part of the dental faculty at the Hebrew University Hadassah Medical School in Jerusalem. There, he completed a concentration in orofacial pain under the mentorship of Dr Yair Sharav and served as chair of the Department of Medicine from 2003 to 2010 before joining the dental school at Rutgers in 2013. Dr Benoliel has published extensively on the subject of orofacial pain, including over 120 articles, book chapters, and case reports. He is also co-editor of the award-winning textbook  The
The