When you hear the term “dermal fillers,” what comes to mind? Are you familiar with the treatment, or is it something you’d like to learn more about? Do you have colleagues who work with dermal fillers? Have you thought about offering them yourself?
After giving courses on dermal fillers for years, Dr Arun Garg has teamed up with Dr Renato Rossi to put together a book on everything dentists need to know about dermal filler treatment: Dermal Fillers for Dental Professionals. In honor of the book’s release, we asked Dr Garg some questions about his experience with fillers and why they’re such a natural extension to dental treatment.
Why did you decide to write a book on dermal fillers?
I’ve been giving courses on dermal fillers, including hands-on workshops on injection techniques, for many years, and a majority of the participants are practicing dentists. Year-over-year attendance at these courses remained steady until about 10 years ago, when I started to see a significant increase in enrollment that has continued until this day (COVID notwithstanding).
People naturally assumed I would have written a book on dermal fillers for dental professionals that they could learn these exciting concepts from. A couple of years ago, after receiving literally hundreds of requests for such a book, I decided to team up with longtime friend and and colleague Dr Renato Rossi to publish our first book on dermal fillers for dentists. Dr Rossi is a highly respected expert on maxillofacial surgery, as well as esthetic facial rejuvenation, and he directs one of the most prestigious academic programs on this topic in all of Brazil, so his contributions to the book are extremely valuable.
How did you get into dermal filler treatment?
This might sound strange, but I see dermal filler and esthetic botulinum toxin therapy as a logical extension of dental implant surgery and reconstruction.
Many of my patients were spending a lot of money to improve their smile only to end up feeling disappointed by the result, because it was framed in thin lips or sagging skin. Minimally invasive facial rejuvenation procedures such as dermal filler injections are the perfect complement to a dental implant and bone grafting smile makeover because (unlike a facelift, for example) the effects are natural and relatively subtle, leaving the patient looking revitalized and refreshed. Today, dermal filler injections generate a significant proportion of my total practice revenue.

How can someone with no experience with fillers, Botox, or microneedling get started with offering these kinds of esthetic treatments to their patients?
The most important is of course getting in reading this book. It is put together in a very logical, systematic, easy to understand, and easy to perform method. Secondly, courses that provide training and instruction in these procedures are available in every major city in the country, but few are tailored to fit the needs of dental practitioners.
Our goal in writing this book was to provide all of the information that dentists need and none of the information that, by virtue of their training, they already possess. But equally important, we present how the various procedures can be successfully and safely incorporated into an existing dental practice using the model that we, as practicing clinical dentists, have developed and taught to hundreds of other dentists over many years.
Why are these kinds of esthetic treatments so perfect for dentists to be providing?
As dentists, or dental specialists, the training and skills make one exceedingly well qualified to provide safe and esthetically pleasing dermal filler injections. Like most dental procedures, administering facial injections for cosmetic purposes requires a combination of strong technical and artistic skills, comprehensive understanding of head and neck anatomy, and knowledge of current biomaterials and treatment modalities. Who is better trained in these areas than dentists and dental specialists? We already have a strong foundation, so why not use it to build some new skill sets?
There are some who may argue that dermal fillers don’t provide any health benefits for patients and are done only for vanity, and therefore not worth the potential risk of complications. How would you convince someone who’s on the fence that the benefits are worth the risk?
 I would say the same thing that I tell my patients when we discuss any type of cosmetic dental treatment: Feeling good about the way you look has nothing to do with vanity. Are there no health benefits to be derived from meditation or yoga, for example, which also help us feel good about ourselves? Veneers, many implant cases, teeth whitening, cosmetic dentistry, and facial rejuvenation, I would argue, are no different than other forms of self-care because the goal is the same: to look and feel better. Just as someone who is ashamed of their smile can suffer from feelings of low self-esteem, depression, social isolation, and so forth, the same is true for the person who has acne scars or signs of premature aging or even thin lips. They feel distressed every time they look in the mirror, and that affects their mood, their personal relationships, and yes, even their health. So I take issue with anyone who tries to argue that dermal fillers don’t provide any health benefits.
I would say the same thing that I tell my patients when we discuss any type of cosmetic dental treatment: Feeling good about the way you look has nothing to do with vanity. Are there no health benefits to be derived from meditation or yoga, for example, which also help us feel good about ourselves? Veneers, many implant cases, teeth whitening, cosmetic dentistry, and facial rejuvenation, I would argue, are no different than other forms of self-care because the goal is the same: to look and feel better. Just as someone who is ashamed of their smile can suffer from feelings of low self-esteem, depression, social isolation, and so forth, the same is true for the person who has acne scars or signs of premature aging or even thin lips. They feel distressed every time they look in the mirror, and that affects their mood, their personal relationships, and yes, even their health. So I take issue with anyone who tries to argue that dermal fillers don’t provide any health benefits.
How would I convince someone who’s on the fence that the benefits of dermal fillers are worth the risk? The short answer is, I wouldn’t. Why? Because I don’t have to! The underlying assumption of this question is that the dentist or dental specialist will have to “sell” this treatment to their patients, but in my opinion that approach is not only wrong-headed but unnecessary. I think many dentists would be pleasantly surprised if they knew how many of their longstanding patients of record have already incorporated some type of professional facial rejuvenation therapy—dermal fillers or Botox or laser skin tightening—into their personal care routine, and would be thrilled to learn that their long-trusted dentist could take over their treatment.
Dentists can introduce cosmetic dermal filler injections as a new service to their patients with virtually no overhead costs other than maintaining an inventory of filler products, and even that can be avoided if they use PRP like I often do. The biggest investment is one they must make in themselves, to expand their knowledge and skill set, and our book contains everything they need to do just that.
Thank you, Dr Garg, for such insightful responses. Preview Drs Garg and Rossi’s new book here, and order your copy today!
 Arun K. Garg, DMD, served as a full-time professor of surgery and director of residency training in the Division of Oral and Maxillofacial Surgery at the University of Miami School of Medicine for nearly 20 years, where he received multiple Faculty Member of the Year awards. He has authored more than a 8 textbooks and over 150 scientific journal articles. He has trained thousands of dentists and dental specialists over the course of his career. Since 2006, he has devoted much of his time and energy to educating and training clinicians on bone grafting and dental implant surgery through Implant Seminars Inc, a company he founded. In addition, he maintains several private practices throughout South Florida. An early adopter and proponent of using dermal fillers and Botox to complement cosmetic dental treatments, in 2011, he cofounded DentaSpa Seminars, which provides education and clinical training in facial rejuvenation procedures designed specifically for dental practitioners.
Arun K. Garg, DMD, served as a full-time professor of surgery and director of residency training in the Division of Oral and Maxillofacial Surgery at the University of Miami School of Medicine for nearly 20 years, where he received multiple Faculty Member of the Year awards. He has authored more than a 8 textbooks and over 150 scientific journal articles. He has trained thousands of dentists and dental specialists over the course of his career. Since 2006, he has devoted much of his time and energy to educating and training clinicians on bone grafting and dental implant surgery through Implant Seminars Inc, a company he founded. In addition, he maintains several private practices throughout South Florida. An early adopter and proponent of using dermal fillers and Botox to complement cosmetic dental treatments, in 2011, he cofounded DentaSpa Seminars, which provides education and clinical training in facial rejuvenation procedures designed specifically for dental practitioners.
 Renato Rossi Jr, DMD, MSc, PhD, is the Dean and Director of the Maxillofacial Residency Program at the Municipal University of São Caetano do Sul in São Paulo, as well as a Professor of Oral and Maxillofacial Surgery at Ibirapuera University in São Paulo. In addition to oral and maxillofacial surgery and traumatology, since 2004, he has also trained his students and residents in maxillofacial esthetics with an emphasis on fillers, advanced techniques in botulinum toxin (Botox), and the use of wires (threads) for facial lifting. To date, he is the author of 8 books, 6 book chapters, and 42 journal articles, and he currently serves as a member of the editorial board of Revista Paulista de Odontologia. Prof Dr Rossi is a Diplomate of the Brazilian College of Maxillofacial Surgery and the International Association of Oral and Maxillofacial Surgeons. He earned a PhD in oral and maxillofacial surgery and traumatology, an MSc in oral pathology, and a DMD from the University of São Paulo.
Renato Rossi Jr, DMD, MSc, PhD, is the Dean and Director of the Maxillofacial Residency Program at the Municipal University of São Caetano do Sul in São Paulo, as well as a Professor of Oral and Maxillofacial Surgery at Ibirapuera University in São Paulo. In addition to oral and maxillofacial surgery and traumatology, since 2004, he has also trained his students and residents in maxillofacial esthetics with an emphasis on fillers, advanced techniques in botulinum toxin (Botox), and the use of wires (threads) for facial lifting. To date, he is the author of 8 books, 6 book chapters, and 42 journal articles, and he currently serves as a member of the editorial board of Revista Paulista de Odontologia. Prof Dr Rossi is a Diplomate of the Brazilian College of Maxillofacial Surgery and the International Association of Oral and Maxillofacial Surgeons. He earned a PhD in oral and maxillofacial surgery and traumatology, an MSc in oral pathology, and a DMD from the University of São Paulo.
 Dermal Fillers for Dental Professionals
Dermal Fillers for Dental Professionals
Arun K. Garg and Renatto Rossi Jr
Have you decided to grow the esthetic side of your dental practice by offering dermal filler treatments? Or do you want to learn a bit more about them before taking the plunge? Esthetic dentistry expert Dr Arun Garg has partnered with Dr Renato Rossi to put together an in-depth clinical manual on everything you need to know to provide dermal filler treatment. The first section covers everything from recommendations for specific filler products to sample patient forms to skin anatomy review. The second section comprises an illustrated step-by-step guide to performing over a dozen specific procedures, categorized by complexity. Each procedure is also accompanied by a real-life case example, and the combination of photographs and computer-generated illustrations provides the reader with the necessary breadth and depth of understanding of every crucial detail to perform these treatments safely and effectively. Whether you’re getting started with dermal fillers and ready to practice the basics or a dermal fillers veteran ready to explore more complex treatments, this book is for you!
208 pp; 645 illus; ISBN: 978-0-86715-830-4 (B8304); $168


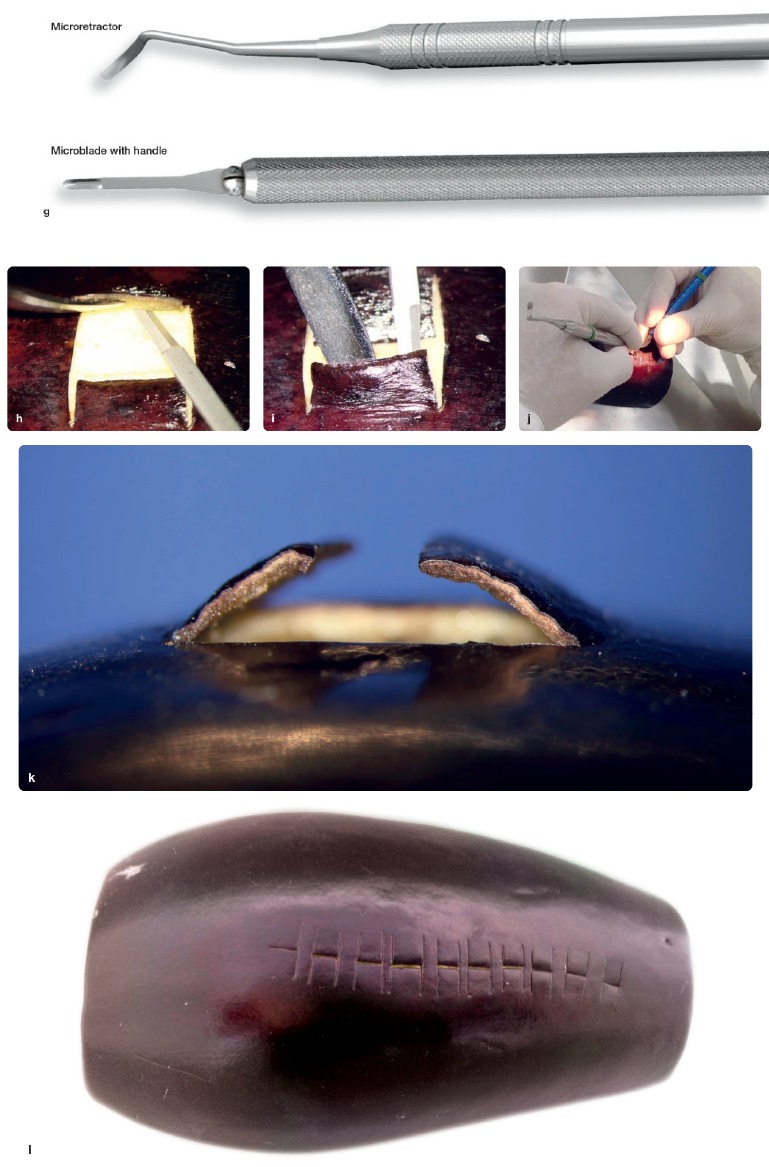
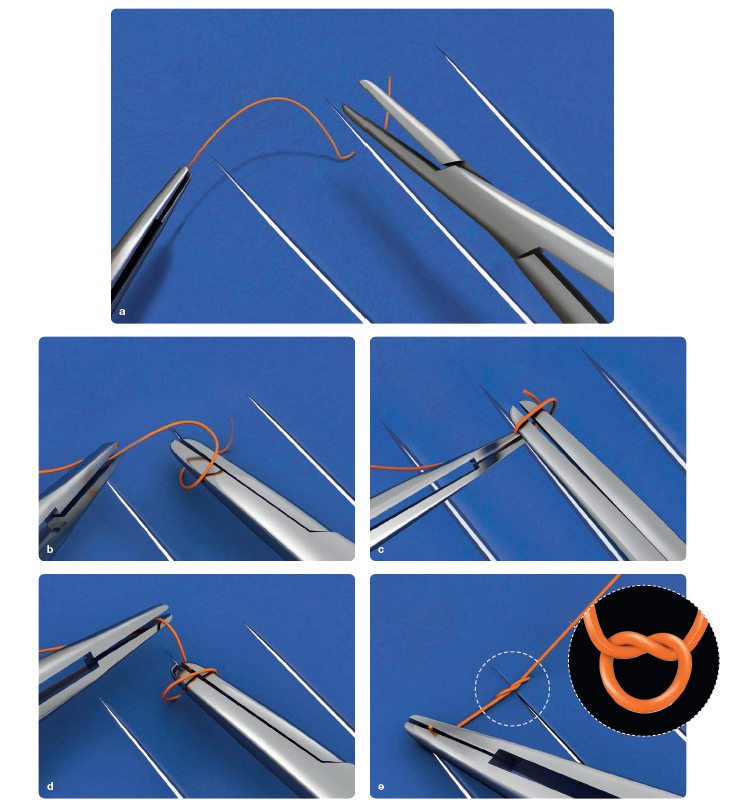
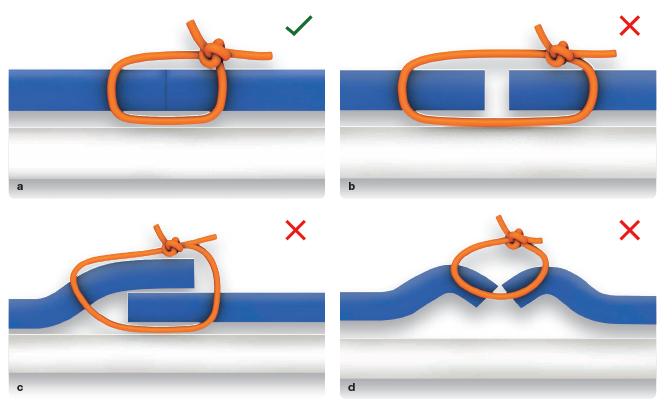
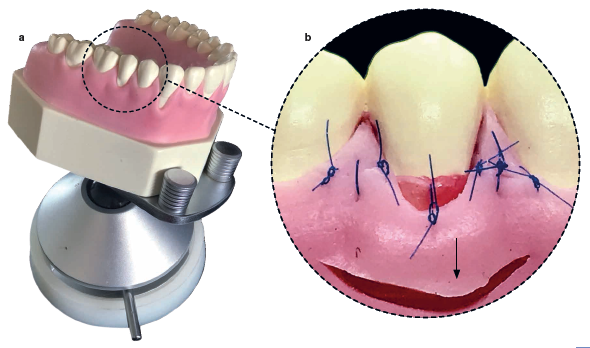
 After the initial development of the skills to perform the root preparations, microincisions, and microsutures, the next step is the study and development of microsurgical techniques for the correction of periodontal and peri-implant defects. Drs Campos and Lopes’s new book illustrates each of these techniques step by step, demonstrated first on a training model and then on a patient in the clinic. Figure 4 above shows the completed S2 technique (two papillae) on the training model. The area of choice for this training is the maxillary second premolar. Figure 5 illustrates the technique on a 48-year-old patient with a 3-mm gingival recession on the maxillary right canine. Surgical planning included approximation microsutures to stabilize the flap and coaptation microsutures for primary wound closure. Figures 5d to 5f show the healing at 5 days, 14 days, and 30 days postoperative, respectively.
After the initial development of the skills to perform the root preparations, microincisions, and microsutures, the next step is the study and development of microsurgical techniques for the correction of periodontal and peri-implant defects. Drs Campos and Lopes’s new book illustrates each of these techniques step by step, demonstrated first on a training model and then on a patient in the clinic. Figure 4 above shows the completed S2 technique (two papillae) on the training model. The area of choice for this training is the maxillary second premolar. Figure 5 illustrates the technique on a 48-year-old patient with a 3-mm gingival recession on the maxillary right canine. Surgical planning included approximation microsutures to stabilize the flap and coaptation microsutures for primary wound closure. Figures 5d to 5f show the healing at 5 days, 14 days, and 30 days postoperative, respectively.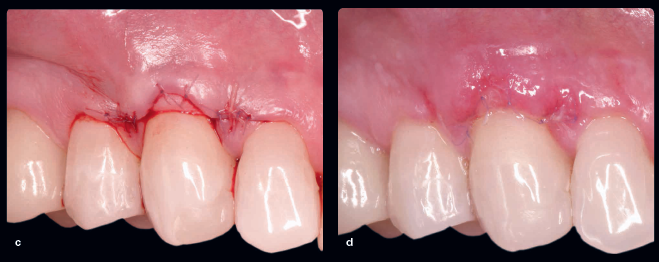
 Root coverage microsurgeries are currently the most common microsurgical procedures performed by periodontists, because there is a high incidence of gingival recession in the population. However, Drs Campos and Lopes consider root coverage procedures to be the most complex microsurgical procedures because “there is often a need to correct the exposed root deformities (noncarious cervical lesions) in order to guide the soft tissue healing process.” Only by following the biologic and surgical principles of the microsurgical philosophy will success be achieved with predictability and long-term outcomes.
Root coverage microsurgeries are currently the most common microsurgical procedures performed by periodontists, because there is a high incidence of gingival recession in the population. However, Drs Campos and Lopes consider root coverage procedures to be the most complex microsurgical procedures because “there is often a need to correct the exposed root deformities (noncarious cervical lesions) in order to guide the soft tissue healing process.” Only by following the biologic and surgical principles of the microsurgical philosophy will success be achieved with predictability and long-term outcomes.
 Glécio Vaz de Campos, DDS, received his DDS degree from the Universidade Estadual Paulista (UNESP) in Araraquara, Brazil, in 1982. After he specialized in periodontics and prosthetics, several years of clinical practice led him to explore new techniques focusing on periodontal plastic surgery. In 1996, he was qualified on this subject at the Microsurgery Training Institute in Santa Barbara, California. He had a significant role in introducing periodontal and peri-implant plastic microsurgery techniques to Brazil and expanding the use of the operative microscope there. From 2000 to 2004, Dr Campos served as Director of the Operative Microscopy Department at the São Paulo Dental Association (APCD), where he organized the largest training facility on operative microscopy in South America. Dr Campos has coauthored 16 books related to periodontal and peri-implant plastic microsurgery, as well as scientific articles published in Brazil and abroad. Currently he maintains private practices in Jundiaí and São Paulo, Brazil, where he focuses on periodontal and peri-implant plastic microsurgery and offers regular training courses in his private microscopy laboratory in Jundiaí.
Glécio Vaz de Campos, DDS, received his DDS degree from the Universidade Estadual Paulista (UNESP) in Araraquara, Brazil, in 1982. After he specialized in periodontics and prosthetics, several years of clinical practice led him to explore new techniques focusing on periodontal plastic surgery. In 1996, he was qualified on this subject at the Microsurgery Training Institute in Santa Barbara, California. He had a significant role in introducing periodontal and peri-implant plastic microsurgery techniques to Brazil and expanding the use of the operative microscope there. From 2000 to 2004, Dr Campos served as Director of the Operative Microscopy Department at the São Paulo Dental Association (APCD), where he organized the largest training facility on operative microscopy in South America. Dr Campos has coauthored 16 books related to periodontal and peri-implant plastic microsurgery, as well as scientific articles published in Brazil and abroad. Currently he maintains private practices in Jundiaí and São Paulo, Brazil, where he focuses on periodontal and peri-implant plastic microsurgery and offers regular training courses in his private microscopy laboratory in Jundiaí. Cláudio Julio Lopes, DDS, received his DDS degree from São Paulo City University in 1989. After specializing in periodontics, he became an assistant professor of periodontics at Camilo Castelo Branco University in Fernandópolis, Brazil, where he stayed from 1990 to 2000. He then moved on to become coordinator of the Periodontal Plastic Surgery and the Introduction to Microsurgery courses at the São Paulo Dental Association, which he continued until 2015. In 2014, he specialized in implantology with the Brazilian Dental Association (ABO), and in 2017, he qualified in reconstructive microsurgery at the Institute of Orthopedics and Traumatology at the University of São Paulo. He maintains a private practice in São Paulo, Brazil.
Cláudio Julio Lopes, DDS, received his DDS degree from São Paulo City University in 1989. After specializing in periodontics, he became an assistant professor of periodontics at Camilo Castelo Branco University in Fernandópolis, Brazil, where he stayed from 1990 to 2000. He then moved on to become coordinator of the Periodontal Plastic Surgery and the Introduction to Microsurgery courses at the São Paulo Dental Association, which he continued until 2015. In 2014, he specialized in implantology with the Brazilian Dental Association (ABO), and in 2017, he qualified in reconstructive microsurgery at the Institute of Orthopedics and Traumatology at the University of São Paulo. He maintains a private practice in São Paulo, Brazil.

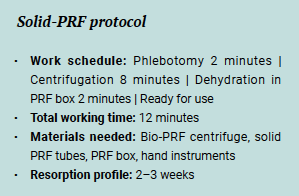 The solid-PRF membrane or plug is created using the horizontal centrifuge and red-cap tubes. The spin time is 700g for 8 minutes, after which a clot is formed. Immediately after centrifugation, the tube lid can be removed to favor clotting via oxygenation. After 5 minutes, the membrane is removed from the tube and the red layer is gently peeled or cut off with scissors, being careful not to cut the buffy coat zone rich in cells (Fig 3). The clot is then transferred to a PRF box, and compression is applied with the PRF box lid (if plugs are desired, cylindric inserts are used to add compression until the piston is flush with the outer rim; Fig 4). Within 2 minutes, the PRF membranes (or plugs) are dehydrated and ready for use. Watch this
The solid-PRF membrane or plug is created using the horizontal centrifuge and red-cap tubes. The spin time is 700g for 8 minutes, after which a clot is formed. Immediately after centrifugation, the tube lid can be removed to favor clotting via oxygenation. After 5 minutes, the membrane is removed from the tube and the red layer is gently peeled or cut off with scissors, being careful not to cut the buffy coat zone rich in cells (Fig 3). The clot is then transferred to a PRF box, and compression is applied with the PRF box lid (if plugs are desired, cylindric inserts are used to add compression until the piston is flush with the outer rim; Fig 4). Within 2 minutes, the PRF membranes (or plugs) are dehydrated and ready for use. Watch this 

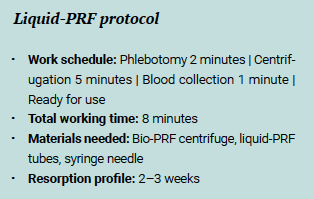 Liquid-PRF is created using a horizontal centrifuge and white- or blue-cap tubes. The spin time is 300g for 5 minutes. The lids should NOT be removed in this case, because oxygenation will speed clotting. An 18G, 1.5-inch syringe needle is used to penetrate the lid of the tube and collect the liquid-PRF. It is important to draw as near to the buffy coat zone as possible and even slightly within this layer (Fig 5). Liquid i-PRF is then ready for injection purposes.
Liquid-PRF is created using a horizontal centrifuge and white- or blue-cap tubes. The spin time is 300g for 5 minutes. The lids should NOT be removed in this case, because oxygenation will speed clotting. An 18G, 1.5-inch syringe needle is used to penetrate the lid of the tube and collect the liquid-PRF. It is important to draw as near to the buffy coat zone as possible and even slightly within this layer (Fig 5). Liquid i-PRF is then ready for injection purposes.
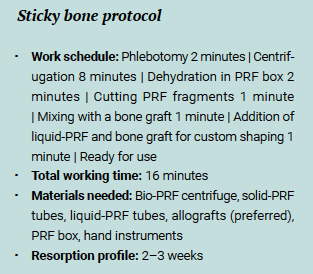 Sticky bone is the term commonly given to the bone graft material with sticky/gummy consistency following the addition of PRF. Two PRF membranes are produced following the solid-PRF protocol, and two tubes of liquid-PRF are also produced following that protocol. The clots are removed from their tubes and cut into small (1-mm) fragments before being mixed with the bone graft material (Fig 6). Only then is the liquid-PRF introduced to the complex to hydrate the entire graft. The sticky bone is then ready for use in bone grafting.
Sticky bone is the term commonly given to the bone graft material with sticky/gummy consistency following the addition of PRF. Two PRF membranes are produced following the solid-PRF protocol, and two tubes of liquid-PRF are also produced following that protocol. The clots are removed from their tubes and cut into small (1-mm) fragments before being mixed with the bone graft material (Fig 6). Only then is the liquid-PRF introduced to the complex to hydrate the entire graft. The sticky bone is then ready for use in bone grafting.
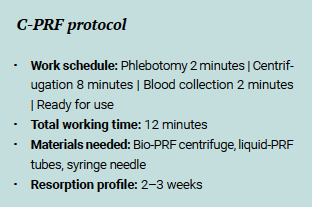 The C-PRF protocol is very similar to the liquid-PRF protocol but it leads to a roughly 10-fold increase in cells and growth factors when compared to whole blood. The spin time is much faster (2000g for 8 minutes), and only the 0.5- to 1-mL layer just above the buffy coat is collected (after discarding the top 3 to 4 mL; Fig 7).
The C-PRF protocol is very similar to the liquid-PRF protocol but it leads to a roughly 10-fold increase in cells and growth factors when compared to whole blood. The spin time is much faster (2000g for 8 minutes), and only the 0.5- to 1-mL layer just above the buffy coat is collected (after discarding the top 3 to 4 mL; Fig 7).
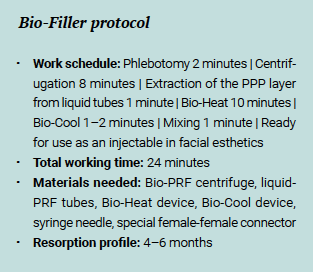 Bio-Filler is fabricated using liquid-PRF tubes spun at 2200g for 8 minutes followed by a Bio-Heat process. From each liquid-PRF tube, the upper 2-mL layer of platelet-poor plasma (PPP) is drawn into a 3-mL syringe and placed in the Bio-Heat device (Bio-PRF) for 10 minutes. After 10 minutes at 75°C, the PPP syringes are placed in the Bio-Cool device (Bio-PRF) for 1 to 2 minutes, while the remaining C-PRF layer in the original tubes is extracted into one syringe per tube. When the albumin gel has cooled down sufficiently, it is mixed back together with the C-PRF layer using 3-mL syringes connected together via a specialized connector. The result is a gel-like texture with extended resorption properties, or e-PRF (Fig 8), which can be used for facial rejuvenation and other facial esthetics procedures.
Bio-Filler is fabricated using liquid-PRF tubes spun at 2200g for 8 minutes followed by a Bio-Heat process. From each liquid-PRF tube, the upper 2-mL layer of platelet-poor plasma (PPP) is drawn into a 3-mL syringe and placed in the Bio-Heat device (Bio-PRF) for 10 minutes. After 10 minutes at 75°C, the PPP syringes are placed in the Bio-Cool device (Bio-PRF) for 1 to 2 minutes, while the remaining C-PRF layer in the original tubes is extracted into one syringe per tube. When the albumin gel has cooled down sufficiently, it is mixed back together with the C-PRF layer using 3-mL syringes connected together via a specialized connector. The result is a gel-like texture with extended resorption properties, or e-PRF (Fig 8), which can be used for facial rejuvenation and other facial esthetics procedures.

 Richard J. Miron, DDS, BMSc, MSc, PhD, Dr med dent, is currently the lead educator and researcher at Advanced PRF Education and is Adjunct Visiting Faculty in the Department of Periodontology at the University of Bern, Switzerland, where he completed his PhD studies. He has published over 250 peer-reviewed articles and lectures internationally on many topics relating to growth factors, bone biomaterials, and guided bone regeneration. Widely considered to be one of the top contributors to research in dentistry, Dr Miron was recognized as the top-ranked researcher on PRF therapy in 2020 according to Expertscape independent review. He also recently won the ITI André Schroeder Prize, the IADR Young Investigator of the Year in the field of implant dentistry, as well as the IADR Socransky Research Award in the field of periodontology. Dr Miron has written five textbooks on regenerative dentistry, and he’s just getting started.
Richard J. Miron, DDS, BMSc, MSc, PhD, Dr med dent, is currently the lead educator and researcher at Advanced PRF Education and is Adjunct Visiting Faculty in the Department of Periodontology at the University of Bern, Switzerland, where he completed his PhD studies. He has published over 250 peer-reviewed articles and lectures internationally on many topics relating to growth factors, bone biomaterials, and guided bone regeneration. Widely considered to be one of the top contributors to research in dentistry, Dr Miron was recognized as the top-ranked researcher on PRF therapy in 2020 according to Expertscape independent review. He also recently won the ITI André Schroeder Prize, the IADR Young Investigator of the Year in the field of implant dentistry, as well as the IADR Socransky Research Award in the field of periodontology. Dr Miron has written five textbooks on regenerative dentistry, and he’s just getting started. Well, we made it to the end of 2020, and I’m sure, like us, you’re ready to say good riddance. But with a new (and hopefully better) year on the horizon, we wanted to look back on the best bits of 2020. After all, despite the pandemic, we’ve released some stellar titles this year. Quintessence has always been committed to clinical excellence, and we take pride in offering our readers the best books in dentistry on the market. We’ve published 15 books this year, and it seems each is more engaging and beautiful than the last.
Well, we made it to the end of 2020, and I’m sure, like us, you’re ready to say good riddance. But with a new (and hopefully better) year on the horizon, we wanted to look back on the best bits of 2020. After all, despite the pandemic, we’ve released some stellar titles this year. Quintessence has always been committed to clinical excellence, and we take pride in offering our readers the best books in dentistry on the market. We’ve published 15 books this year, and it seems each is more engaging and beautiful than the last.

 Another 10 years of developments in GBR, another new edition of this title. Once again, the top names in regenerative dentistry have come together to bring you the latest evidence-based practices in GBR. With elements of literature review combined with a clinical manual, this seminal text is a must-have for implantologists.
Another 10 years of developments in GBR, another new edition of this title. Once again, the top names in regenerative dentistry have come together to bring you the latest evidence-based practices in GBR. With elements of literature review combined with a clinical manual, this seminal text is a must-have for implantologists. Orthognathic surgery should NOT be reserved only for when orthodontics fails or is insufficient. This revolutionary title explores the primacy of orthognathic surgery in treatment planning for patients with small jaws (and the almost inevitable compressed airways that come with them), detailing six surgical methods to design a face to permit patients to breathe normally, eat normally, speak normally, and function normally in society.
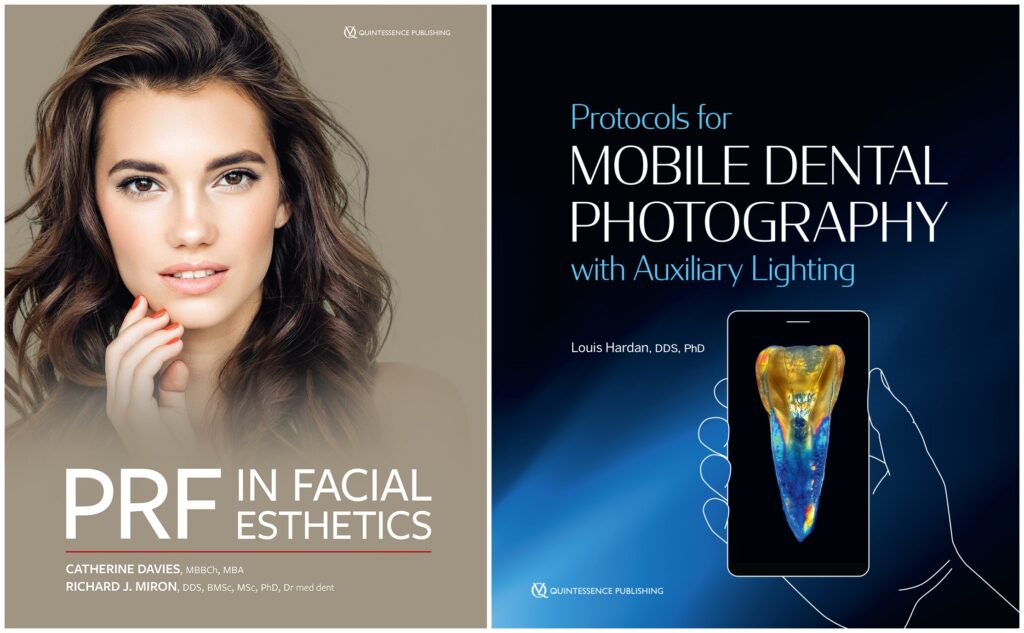
Orthognathic surgery should NOT be reserved only for when orthodontics fails or is insufficient. This revolutionary title explores the primacy of orthognathic surgery in treatment planning for patients with small jaws (and the almost inevitable compressed airways that come with them), detailing six surgical methods to design a face to permit patients to breathe normally, eat normally, speak normally, and function normally in society. Fillers have exploded in popularity in the last few years, and for good reason. This book is geared toward practitioners who are ready to take the plunge and begin offering these cosmetic treatments to their patients. Beginning with important background info on fillers and ending with step-by-step instructions for a dozen different procedures, this text will guide you on your journey from novice to expert with administering fillers.
Fillers have exploded in popularity in the last few years, and for good reason. This book is geared toward practitioners who are ready to take the plunge and begin offering these cosmetic treatments to their patients. Beginning with important background info on fillers and ending with step-by-step instructions for a dozen different procedures, this text will guide you on your journey from novice to expert with administering fillers. Simplicity is the goal of this very different style of book. Dr Hirata views his techniques as recipes and organizes them in the format of a cookbook. What a clear and concise way to present this valuable material! We’re excited about this one!
Simplicity is the goal of this very different style of book. Dr Hirata views his techniques as recipes and organizes them in the format of a cookbook. What a clear and concise way to present this valuable material! We’re excited about this one! When we say “complete,” we’re not kidding! This expansive textbook has all the topics covered in periodontal exams, organized in an easy-to-read format with dozens of tables, diagrams, illustrations, and vocabulary words to supplement the text. But it’s more than just exam review—even periodontists who have already begun practice will find it an invaluable tool in their careers.
When we say “complete,” we’re not kidding! This expansive textbook has all the topics covered in periodontal exams, organized in an easy-to-read format with dozens of tables, diagrams, illustrations, and vocabulary words to supplement the text. But it’s more than just exam review—even periodontists who have already begun practice will find it an invaluable tool in their careers. Post and core is an invaluable and underutilized technique for saving teeth. Extraction is sometimes the only option, but it should not be the first choice. This book reviews how advancements in technology in varying fields of dentistry can come together and provide endodontic solutions for complex clinical scenarios. Beautiful and intricate case studies demonstrate the different applications and techniques Dr Terry uses to restore the intraradicular post space in his patients.
Post and core is an invaluable and underutilized technique for saving teeth. Extraction is sometimes the only option, but it should not be the first choice. This book reviews how advancements in technology in varying fields of dentistry can come together and provide endodontic solutions for complex clinical scenarios. Beautiful and intricate case studies demonstrate the different applications and techniques Dr Terry uses to restore the intraradicular post space in his patients.