Reading time: 9 minutesWritten by: Marieke Zaffron
With the rise of platforms like Instagram and all the photos of young, beautiful people—edited or not—that come with it, it’s no surprise that demand for cosmetic treatments is at an all-time high, with no sign of slowing down. Fortunately, the technologic developments that enable increased exposure to sometimes unachievable beauty standards have been accompanied by technologic developments in the fields of esthetics and dermatology, making treatments to combat aging safer than ever before.
Now you—and your patients—may be asking, what do skin treatments have to do with dental treatment? Why are dentists offering things like Botox? Shouldn’t that be left to dermatologists?
The fact is that dentists are remarkably well-equipped to deal with procedures affecting the skin of the face. Many of the lines and wrinkles that patients most want to minimize occur around the mouth, and who has a better understanding of the anatomy in this area than dentists? Dentists are very familiar with administering anesthesia, and many have already used adjunctive products like platelet-rich plasma (PRP), platelet-rich fibrin (PRF), and hyaluronic acid (HA) for other applications.
Dentists are remarkably well-equipped to deal with procedures affecting the skin of the face.
When we perform prosthetic treatment planning, we consider the face as a whole. It’s not just the teeth, but the smile. It’s not just the smile, but the face. Asking patients what they would like to change about the esthetics of their smile provides an opportunity to discuss the face as a whole. Patients may be unaware that things such as wrinkles, scars (including acne scars), and more can be treatable at the dentist’s office, often for a relatively low cost, with a low risk of complications, and with great success.
Microneedling in particular, which is discussed in both Drs Catherine Davies and Richard Miron’s PRF in Facial Esthetics and Drs Arun Garg and Renato Rossi’s upcoming Dermal Fillers for Dental Professionals, has many advantages compared with other treatments. As Drs Garg and Rossi explain, “Dermal microneedling restores firmness and elasticity to the face. It has become a popular alternative to more invasive procedures such as laser skin resurfacing and deep chemical peeling for skin rejuvenation. It is noninvasive and does not damage the skin, and it can be performed using topical anesthesia, another feature that is attractive to patients.” Drs Davies and Miron add that the healing time for this method is shorter than other options (only 1 to 2 days), is appropriate for all skin types, and is well tolerated by patients. The procedure is also quick to perform in office—15 to 20 minutes—and is easy to master.
How Microneedling Works
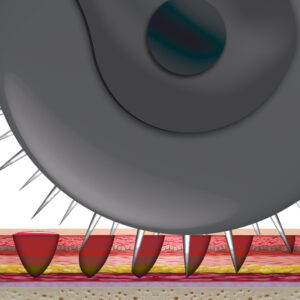 Microneedling is a minimally invasive treatment that involves using a specialized tool such as a roller or a pen to make tiny puncture wounds on the surface of the skin—approximately 200 punctures per square centimeter, according to Drs Garg and Rossi. Because it is technically an injury, the body responds with wound-healing processes, including the release of growth factors. As Drs Davies and Miron explain, “Microneedling induces soft tissue fibroblast proliferation and collagen and extracellular matrix deposition, re-epithelialization, and angiogenesis. … It has also been shown to stimulate collagen production by creating microchannels into the dermis and initiating a repair process.” Importantly, scars will not form as a result of microneedling. The injury is controlled and minimal, just enough for neocollagenesis to produce new collagen and elastin to tighten the skin and improve its architecture.
Microneedling is a minimally invasive treatment that involves using a specialized tool such as a roller or a pen to make tiny puncture wounds on the surface of the skin—approximately 200 punctures per square centimeter, according to Drs Garg and Rossi. Because it is technically an injury, the body responds with wound-healing processes, including the release of growth factors. As Drs Davies and Miron explain, “Microneedling induces soft tissue fibroblast proliferation and collagen and extracellular matrix deposition, re-epithelialization, and angiogenesis. … It has also been shown to stimulate collagen production by creating microchannels into the dermis and initiating a repair process.” Importantly, scars will not form as a result of microneedling. The injury is controlled and minimal, just enough for neocollagenesis to produce new collagen and elastin to tighten the skin and improve its architecture.
Who Can Benefit
Microneedling began as a treatment for wrinkles, but it now has multiple indications, including wrinkles, stretch marks, hair loss, hyperpigmentation, ultraviolet damage, acne, and scars (including acne scars). There are, however, some contraindications to microneedling. Microneedling has been shown to be less effective on ice pick scars than other types of atrophic scars. Patients taking blood thinners should not undergo microneedling therapy because of an increased risk of bleeding. (Though the procedure ordinarily results in very minimal bleeding.) Diseases of the skin such as eczema, rosacea, and malignancies are further contraindications.
However, most patients who have undergone microneedling have been very happy with the results. Studies have shown microneedling to be very effective in the treatment of wrinkles as well as most types of atrophic scars, with patients reporting great improvements and high levels of satisfaction. In addition, because the needles are varying sizes—0.2 to 3.0 mm—they can even be used in sensitive areas such as around the eyes and lips if a shorter needle is chosen.
Studies have shown microneedling to be very effective in the treatment of wrinkles as well as most types of atrophic scars, with patients reporting great improvements and high levels of satisfaction.
Microneedling Options

The two main methods of microneedling include using a pen and using a roller. Each of these categories includes many different products with a wide variety of options, settings, and needle lengths. Drs Davies and Miron recommend the Dermapen, a pen with disposable needles whose size can be adjusted as necessary during treatment. As they explain, “The Dermapen is an electrically powered medical device that delivers a vibrating stamplike motion to the skin, resulting in a series of microchannels.” Drs Garg and Rossi, on the other hand, recommend using a roller: “Because of the action of the roller, the needle penetrates the skin at an angle and then goes deeper as the roller turns.”
Microneedling Procedure
The microneedling procedure itself is actually quite simple, especially when compared with procedures utilizing dermal fillers or botulinum toxin, which require precise injections into very specific areas of the face. Topical anesthesia is applied to the face, and the clinician waits for the anesthesia to take effect. The specific application method of the microneedles will depend on the type of device chosen and the area of the face to be treated.

After the procedure, topical adjuncts such as PRP, PRF, or HA can be applied to the area. Because of the microchannels created in the skin, it is extremely receptive to the beneficial healing properties of these products at this time.
Side effects of the procedure are very mild. Any bleeding that occurs during the procedure should stop very quickly. There may be bruising and erythema that can last a few days. Depending on the severity of the patient’s condition, additional treatments may be required, but patients should wait 1 to 2 months before undergoing an additional microneedling procedure.
Comparison with At-Home Treatment
One unique aspect of microneedling is that it is a procedure that can be performed at home by patients themselves as well as by medical professionals. Of course, the two treatments are quite different. As Drs Garg and Rossi point out, “The key difference in these devices is the length of the needles. Most consumer models have needles of 0.2 to 0.3 mm in length. Medical-grade dermal needling devices have needles ranging from 0.2 mm up to 3.0 mm because they are designed to treat specific conditions.” Dermal rollers are available for purchase for as little as $10 or less, while medical-grade devices cost in the hundreds or thousands of dollars range. Clearly, one of these devices will be more effective than the other.
While the shorter needles of consumer microneedling products ensure that they carry less risk than with longer needles, the fact remains that the skin is being punctured by a user with less knowledge of facial anatomy, who may be using more or less force than is recommended, and who is likely not working with sterile equipment and in a sterile environment. In addition, at-home procedures may be more painful for the patient because they will be performed without anesthesia. Also, patients will not have access to adjuncts such as PRP, PRF, or HA to apply to the skin afterward. There are many topical products that consumers can use after an at-home microneedling procedure, but because these will go deeper into the skin than normal, it is necessary for patients to educate themselves on what products are safe and which may be harmful.
Conclusion
The more dentists who begin offering microneedling procedures as part of their practice, the more patients who can benefit.
Overall, while at-home treatment may be a good alternative for patients on a tight budget and who desire nothing more than a simple refresh of the skin, those who want more significant results will seek out professional treatment. The more dentists who begin offering microneedling procedures as part of their practice, the more patients who can benefit. Patients who have already been seeing you for years may feel more comfortable undergoing this treatment with someone they already trust rather than finding a new practitioner. Also, because even medical-grade microneedling is a simpler procedure to learn and perform than dermal fillers or botulinum toxin injections, it is a perfect “beginner” cosmetic procedure for clinicians considering expanding their practice. What better way is there to test the waters and find out whether including more cosmetic treatments would be right for you and your patients than to start with something small and simple? Microneedling is often used as an adjunct to dermal fillers, and dermal fillers may be used as an adjunct to Botox, so if you expand your practice further, your microneedling patients may become your first advanced cosmetic procedure patients.
Are you ready to take the next step? These new and forthcoming cosmetic dentistry titles are a great place to start:
 Dermal Fillers for Dental Professionals
Dermal Fillers for Dental Professionals
Arun K. Garg and Renato Rossi, Jr
Esthetic medical procedures have evolved from the invasive, complex face-lift surgeries of the past to the modern practice of minimally invasive injections of dermal fillers, neurotoxins, and autologous agents. This book introduces these techniques and explains how to choose the most appropriate method for the situation, then provides precise instructions on how to administer different treatments. Photographic and illustrated diagrams explicitly demonstrate both the “where” and the “how” of the facial injection techniques, so clinicians can feel confident about applying these protocols and discovering the impressive results that will make patients feel most comfortable in their skin.
Coming soon! Join our mailing list for updates!
 PRF in Facial Esthetics
PRF in Facial Esthetics
Edited by Catherine Davies and Richard J. Miron
Written in collaboration with international experts from various fields of medicine, including basic scientists, clinician-scientists, experts in laser therapy and photography, as well as plastic surgeons and hair restorative surgeons, this book collectively offers a comprehensive approach to using platelet-rich fibrin (PRF) in facial esthetics. PRF has been used for decades in regenerative medicine, and slowly it has made its way into the medical esthetic arena, often used in combination with other leading therapies to support minimally invasive esthetic procedures. This book therefore starts at the beginning, first exploring the biology and anatomy of the skin and hair before turning to clinical chapters on patient consultation, microneedling, skin and hair regeneration, lasers, and the use of PRF in plastic surgery. The final chapter looks to the future and considers what else could be possible. If you perform any facial esthetic procedures in your office or want to learn how, this book is a must.
248 pp; 380 illus; ©2020; ISBN 978-0-86715-957-8 (B9578); $168
 Dermal Fillers for Facial Harmony
Dermal Fillers for Facial Harmony
Altamiro Flávio
In our esthetics-obsessed culture, patients are becoming more aware and demanding of dermal filler treatments. Yet all too often we hear news stories of botched procedures or anesthesia gone wrong. This book walks you through how to incorporate dermal fillers into your clinical armamentarium, starting with the basic characteristics of the materials and advancing to the injection techniques and clinical indications for their use. The author includes such fine detail as whether to use a needle versus a cannula and why you must understand the precise tissue layers of the face in order to effectively deliver this nuanced treatment. In step with its sister volume, Botulinum Toxin for Facial Harmony, the book focuses on facial analysis as a crucial step in determining appropriate treatment, a philosophy that is carried through the entire book. An entire chapter is devoted to clinical cases illustrating the various facial regions and their appropriate filler applications, clearly demonstrating how to use the techniques presented to optimize esthetics and facial harmony. Supplemental material and videos are available via QR code for additional learning.
176 pp; 228 illus; ©2019; ISBN 978-0-86715-821-2 (B8212); US $148
 Botulinum Toxin for Facial Harmony
Botulinum Toxin for Facial Harmony
Altamiro Flávio
This book shows practitioners how to address facial asymmetries with clinical Botox therapy. The book covers comprehensive facial analysis and how to plan treatment. Injection points are identified within a larger discussion of anatomical considerations, and detailed treatment instructions include dosage, syringe type, and needle size for each clinical procedure as well as how to evaluate the results. This stunning book will widen the esthetic treatment options you can provide for patients.
160 pp; 359 illus; ©2018; ISBN 978-0-86715-787-1 (B7871); US $148







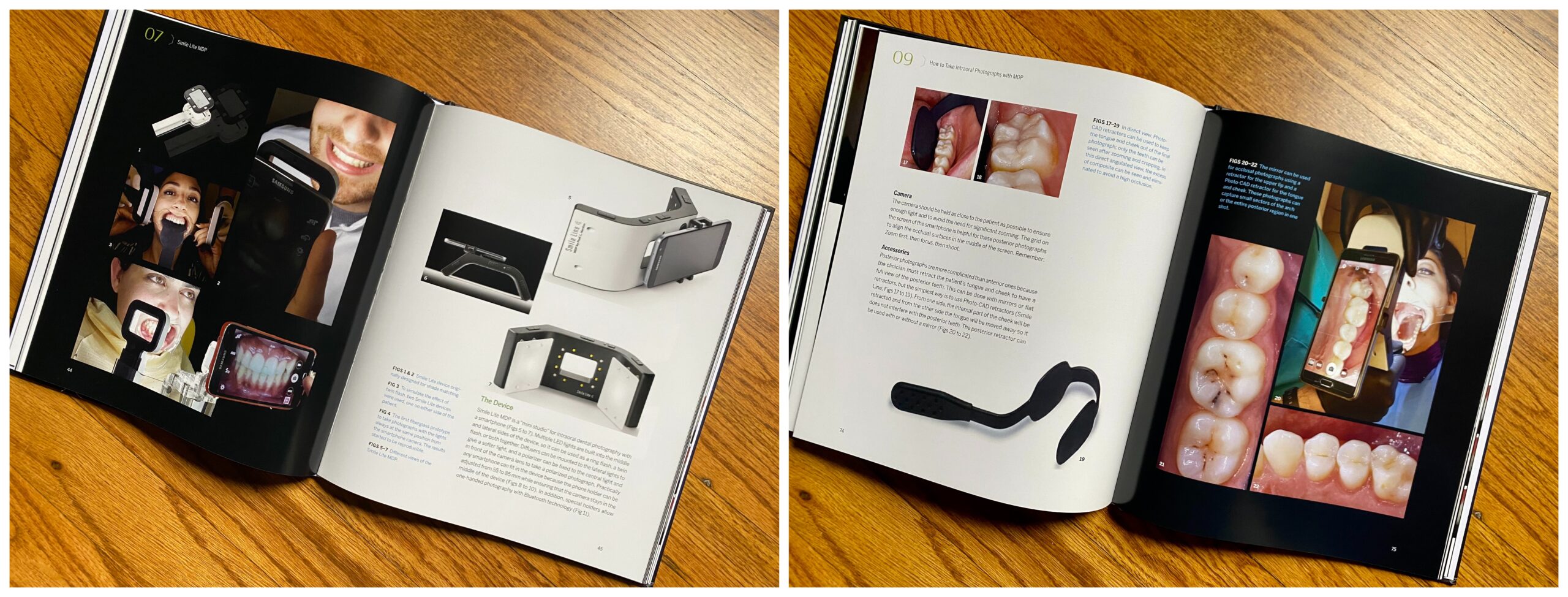


 Dr Hardan wants dentists to be excited about MDP for its many advantages: “Every dentist has a free camera in his pocket with high performance. Since photography is a good management of light, MDP will offer to the dentist a mini studio where he has all kinds of light used in professional photography, from the ring flash and lateral flashes to diffused and polarized light. Since the light is continuous, the user can see on his screen the final result before taking the picture.” Better yet is that this system costs way less than a professional-grade DSLR camera and is way more intuitive to use.
Dr Hardan wants dentists to be excited about MDP for its many advantages: “Every dentist has a free camera in his pocket with high performance. Since photography is a good management of light, MDP will offer to the dentist a mini studio where he has all kinds of light used in professional photography, from the ring flash and lateral flashes to diffused and polarized light. Since the light is continuous, the user can see on his screen the final result before taking the picture.” Better yet is that this system costs way less than a professional-grade DSLR camera and is way more intuitive to use. One of the coolest things about MDP is that you can use it to take artistic photographs like half-illuminated portraits, birefringence photographs, and glam shots of lips and teeth. Dr Hardan shows in his book how to take all of these with your smartphone. Social media has quickly become an effective marketing tool for dentists, and shots like these can give you the edge you need to succeed. As Dr Hardan underscores, “Lots of pictures on social media are low quality because of the lighting used. High-quality photographs with MDP can be used to market our work. If the dental treatment is perfect but the pictures are bad in quality, the marketing message will be very bad. That is why the dental pictures should be perfect, and by adding artistic pictures, the impact on social media will be very high.”
One of the coolest things about MDP is that you can use it to take artistic photographs like half-illuminated portraits, birefringence photographs, and glam shots of lips and teeth. Dr Hardan shows in his book how to take all of these with your smartphone. Social media has quickly become an effective marketing tool for dentists, and shots like these can give you the edge you need to succeed. As Dr Hardan underscores, “Lots of pictures on social media are low quality because of the lighting used. High-quality photographs with MDP can be used to market our work. If the dental treatment is perfect but the pictures are bad in quality, the marketing message will be very bad. That is why the dental pictures should be perfect, and by adding artistic pictures, the impact on social media will be very high.”
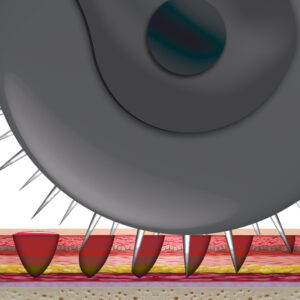 Microneedling is a minimally invasive treatment that involves using a specialized tool such as a roller or a pen to make tiny puncture wounds on the surface of the skin—approximately 200 punctures per square centimeter, according to Drs Garg and Rossi. Because it is technically an injury, the body responds with wound-healing processes, including the release of growth factors. As Drs Davies and Miron explain, “Microneedling induces soft tissue fibroblast proliferation and collagen and extracellular matrix deposition, re-epithelialization, and angiogenesis. … It has also been shown to stimulate collagen production by creating microchannels into the dermis and initiating a repair process.” Importantly, scars will not form as a result of microneedling. The injury is controlled and minimal, just enough for neocollagenesis to produce new collagen and elastin to tighten the skin and improve its architecture.
Microneedling is a minimally invasive treatment that involves using a specialized tool such as a roller or a pen to make tiny puncture wounds on the surface of the skin—approximately 200 punctures per square centimeter, according to Drs Garg and Rossi. Because it is technically an injury, the body responds with wound-healing processes, including the release of growth factors. As Drs Davies and Miron explain, “Microneedling induces soft tissue fibroblast proliferation and collagen and extracellular matrix deposition, re-epithelialization, and angiogenesis. … It has also been shown to stimulate collagen production by creating microchannels into the dermis and initiating a repair process.” Importantly, scars will not form as a result of microneedling. The injury is controlled and minimal, just enough for neocollagenesis to produce new collagen and elastin to tighten the skin and improve its architecture.

 Dermal Fillers for Dental Professionals
Dermal Fillers for Dental Professionals