Reading time: 8 minutesWritten by: Natalie Schawel
The term treatment planning means to plan a sequence of procedures to provide a solution (or treatment) for a previously identified problem (or diagnosis). Simple enough, right? Not really. “Unfortunately, treatment planning is always implied but never formally taught,” says Dr Antonio H.C. Rodrigues, DDS, MScD, author of Treatment Planning in Restorative Dentistry and Implant Prosthodontics. “Consequently, only a segmented view of the patient’s condition is presented, which may compromise treatment results in the long term.”
“Unfortunately, treatment planning is always implied but never formally taught,” says Dr Antonio H.C. Rodrigues.
Comprehensive treatment planning, on the other hand, allows for total care, which involves treating the entirety of a patient’s situation rather than relying on siloed expertise and addressing problems as they arise. But how are clinicians supposed to learn how to treatment plan like this if they are never taught?
A lack of understanding of how to approach treatment planning is severely detrimental to educators, students, and practicing dentists. As Dr Rodrigues explains, “Most complications and failures, particularly in restorative dentistry, are directly or indirectly related to inadequate planning. When planning procedures are not carried out accordingly, dentists tend to provide either overtreatment or undertreatment for their patients. Either situation may cause problems in the long term.” In the end, poor treatment planning can significantly diminish a treatment’s effectiveness and success, negatively impacting a patient’s experience as well as their outcomes.
Learning from historical and contemporary approaches
To understand the benefits of comprehensive treatment planning, one must first look to the past. Dentists are undoubtedly content to see previous philosophies stay in the past, such as empirically driven decisions or focusing treatment on just one problem, like pain or a missing tooth. For instance, a patient might complain about poor esthetics and functioning of a denture, leading them to request an implant-supported restoration. In an effort to oblige the patient, the dentist may comply—without considering reduced space in the mouth or the reduced number of posterior teeth. As a result of an incomplete examination, and thus an incomplete plan, the future implant-supported prosthesis may endure excessive occlusal forces and, ultimately, fail.
In the past, patients also lacked treatment options—or were never provided enough information to make an informed decision. Once patients did choose an option, dentists often moved forward using segmented planning steps and siloed approaches that did not incorporate other areas of expertise. Historical philosophies compromised treatment after treatment, and it was a welcome move to enter a more contemporary school of thought.
Contemporary planning concepts
Modern dentistry brought new knowledge and new implications. “Making a diagnosis and planning a treatment implies the professional responsibility to omit nothing of consequence for the patient; deviation of this line of thought has become unacceptable and is no longer tolerated,” explains Dr Rodrigues. New diagnostic instruments have led to improved accuracy and predictability. Dentists can now refer to concrete evidence to make decisions rather than solely their own experience, which is an essential factor in the treatment-planning process. Finally, patient-dentist conversations have become more productive as dentists provide patients with thorough information about their individual situation during the planning process. And when it comes time for treatment, advancements in research have led to more sophisticated treatment options.
Though great strides have been made in treatment planning, a gaping hole remains, which threatens the success of treatments, patient satisfaction, and dentistry as a whole. This is where comprehensive treatment planning comes in—offering an option to consider patients in their entirety from very initial procedures to final treatments and outcomes.
Comprehensive treatment planning: From a segmented approach to a seamless one
Contemporary planning concepts should not be completely abandoned; rather, they should be nicely folded into an approach that considers the patient as a whole throughout the entire process.
This requires access to important information for the profession at large, according to Dr Lino Calvani, MD, DDS, CDT, MSc, PhD, author of Fundamentals of Treatment Planning: Guidelines on How to Develop, Plan, Write, and Deliver a Prosthodontic Care Project. This information can guide students and practitioners, helping them better care for their patients.
Gone are the days when dentists can remain focused on the contents of their own specialties.
To begin with, treatment planning should be grounded in a holistic view. Gone are the days when dentists can remain focused on the contents of their own specialties. By focusing on one area of expertise—which is often connected to a patient’s primary complaint—important information may go completely ignored. On the other hand, by dutifully considering all areas of expertise during treatment planning, the entire treatment promises to be more successful and stable in the long term.
With this in mind, comprehensive treatment planning also lends itself to certain principles in order to gather all pertinent information. These include how the patient presents for examination, their original healthy state, and the ideal outcome for the patient’s individual situation. Understanding a patient’s existing condition alongside their original healthy condition allows a clinician to accurately—and holistically—determine a realistic, ideal approach. In the end, knowledge of the problem, the solution, and any treatment modifiers is key to formulating a thorough, successful treatment plan.
Including the patient in treatment planning
Originally, treatment plans were intended just to provide guidance for delivering treatment. At first glance, this doesn’t sound terribly far off from a holistic, effective approach. However, treatment plans are not comprehensive if they do not involve the patient. As a part of treatment planning, patients should be counseled about their condition and what methods are available to solve their problems. Meanwhile, this process can be utilized to obtain informed consent. In its entirety, the goals of treatment planning include developing a comprehensive treatment plan, educating the patient, and obtaining consent from the patient.
In its entirety, the goals of treatment planning include developing a comprehensive treatment plan, educating the patient, and obtaining consent from the patient.
Approaching treatment planning with planning phases
From tooth preparation to implant surgery, dental procedures often come with sequence protocols, which are modifiable steps to ensure a process’s predictability. Yet treatment planning has historically been approached without similar protocols. However, these protocols would provide much-needed assistance from initial consultations to the final treatment plan presentation.
Dr Rodrigues separates these protocols into four phases:
- Data gathering and problem identification
- Interpretation of data and diagnosis, prognosis, and objectives
- Analysis of treatment options and development of a treatment plan
- Patient education and informed consent

Dr Calvani similarly separates the treatment-planning process into three distinct phases:
- Diagnostics
- Improvement, disease, restorative
- Maintenance

For both Dr Rodrigues and Dr Calvani, the goals of each phase must be achieved in order for the protocols to be effective. For instance, accurate data is necessary for efficiency in diagnosis. This may require tools, such as checklists or questionnaires, to assist the clinician in gathering of data.

In addition, while protocols remain flexible in that they are continually modified to adapt to the increasing pool of knowledge of an experienced clinician, it is critical to focus on each phase individually.
From identified problems to proposed solutions, treatment planning is a robust endeavor, and overlooking important steps of treatment planning may lead to complications and treatment failures down the road. However, if approached with careful consideration and methodology, patient outcomes and satisfaction can be significantly improved.


If you want to improve your treatment planning and achieve better and more predictable outcomes, check out Dr Calvani’s and Dr Rodrigues’s new books. Preview the first chapter of each book below.
Preview: Treatment Planning in Restorative Dentistry and Implant Prosthodontics by Antonio H.C. Rodrigues
Preview: Fundamentals of Treatment Planning: Guidelines on How to Develop, Plan, Write, and Deliver a Prosthodontic Care Project by Lino Calvani
 Treatment Planning in Restorative Dentistry and Implant Prosthodontics
Treatment Planning in Restorative Dentistry and Implant Prosthodontics
Antonio H.C. Rodrigues
Treatment planning is commonly considered one of the most important phases of any dental treatment and vital for achieving successful long-term results. However, most dental schools do not offer courses exclusively designed for comprehensive planning, and comprehensive planning is rarely discussed at scientific meetings because it is considered a basic topic that practitioners should already understand. This knowledge gap leaves practicing clinicians with few options beyond using their own intuition to solve problems, which is highly unpredictable. Therefore, this book presents clinical guidelines for planning treatments in restorative dentistry and outlines a clear, objective, and simple thinking process that can be easily applied in daily practice, essentially providing the reader with a roadmap to be used as a reference from the very initial procedures until final restorative treatment. Part 1 describes how to identify existing problems by gathering, organizing, and analyzing information obtained during clinical examination. Examination checklists and forms are included to ensure that no important information is left out during the evaluation process. Part 2 focuses on providing solutions to identified problems via restorative treatment options, highlighting the use of implant-supported restorations in the treatment of both partially and completely edentulous arches. Part 3 details how to present treatment options to the patient and includes aspects related to patient education, treatment plan presentation, and obtaining informed consent from the patient. Altogether, this book will transform the way you treatment plan your cases.
 Fundamentals of Treatment Planning: Guidelines on How to Develop, Plan, Write, and Deliver a Prosthodontic Care Project
Fundamentals of Treatment Planning: Guidelines on How to Develop, Plan, Write, and Deliver a Prosthodontic Care Project
Lino Calvani
This book is a comprehensive prosthodontic treatment guide that outlines and explains the various aspects and possibilities of medical and dental treatment planning as it exists today. The content is logically organized in a step-by-step manner and addresses a wide audience: prosthodontic specialists, graduates and postgraduate students, general practitioners, and specialists in other dental fields. Topics include the goals of treatment planning, prosthodontic tools, first meeting with the patient, diagnostics and prognostics, intraoral and extraoral physical examination, types and structure of prosthodontic treatment, the writing of a treatment plan, and more. All clinicians who organize prosthetic and reconstructive treatments in their daily work will benefit from this book.


 Tooth-Preserving Surgery
Tooth-Preserving Surgery

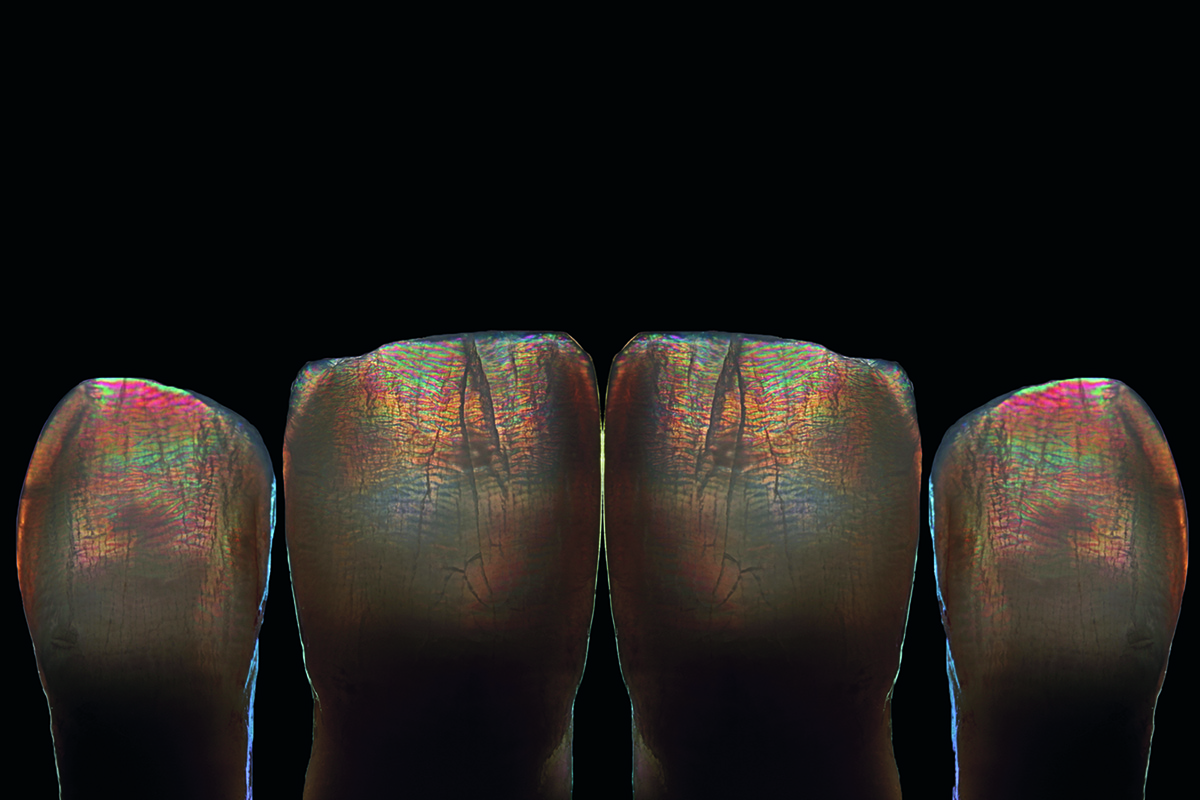

 Sillas Duarte, Jr, DDS, MS, PhD, is the Rex Ingraham Chair in Restorative Dentistry, Associate Professor and Chair, Division of Restorative Sciences, and Director of the Advanced Dental Education Program in Operative Dentistry, Ostrow School of Dentistry of University of Southern California, Los Angeles, California. In addition to his 12 years as editor-in-chief of QDT, Dr Duarte serves as co-chair of the International Symposium on Ceramics, sponsored by Quintessence Publishing every 3 years. He lectures and conducts hands-on courses nationally and internationally, teaching cutting-edge clinical techniques and technologies related to esthetic and adhesive dentistry. His research and clinical work focus on bonding to dental structures, composites, and ceramics.
Sillas Duarte, Jr, DDS, MS, PhD, is the Rex Ingraham Chair in Restorative Dentistry, Associate Professor and Chair, Division of Restorative Sciences, and Director of the Advanced Dental Education Program in Operative Dentistry, Ostrow School of Dentistry of University of Southern California, Los Angeles, California. In addition to his 12 years as editor-in-chief of QDT, Dr Duarte serves as co-chair of the International Symposium on Ceramics, sponsored by Quintessence Publishing every 3 years. He lectures and conducts hands-on courses nationally and internationally, teaching cutting-edge clinical techniques and technologies related to esthetic and adhesive dentistry. His research and clinical work focus on bonding to dental structures, composites, and ceramics.
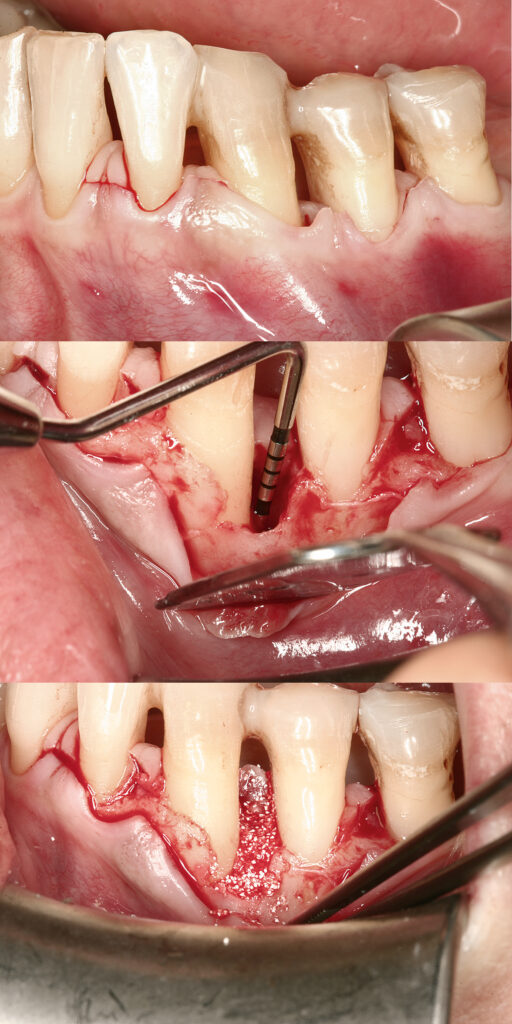
 Leonardo Trombelli, DDS, PhD, is the chair of the Periodontology Department at the University of Ferrara in Ferrara, Italy. He was Dean of the University of Ferrara Dental School from 2013 to 2018 and President of the Dental School from 2014 to 2016. Dr Trombelli is also a Past President of the Italian Society of Osseointegration and an Active Member of the Italian Society of Periodontology, the Italian Academy of Osseointegration, and the International Association for Dental Research. He serves as editorial board member for the Journal of Clinical Periodontology and Journal of Dental Research, and he is also a member of the peer-review panel for the Journal of Periodontology. Dr Trombelli also maintains a private practice limited to periodontology and oral surgery.
Leonardo Trombelli, DDS, PhD, is the chair of the Periodontology Department at the University of Ferrara in Ferrara, Italy. He was Dean of the University of Ferrara Dental School from 2013 to 2018 and President of the Dental School from 2014 to 2016. Dr Trombelli is also a Past President of the Italian Society of Osseointegration and an Active Member of the Italian Society of Periodontology, the Italian Academy of Osseointegration, and the International Association for Dental Research. He serves as editorial board member for the Journal of Clinical Periodontology and Journal of Dental Research, and he is also a member of the peer-review panel for the Journal of Periodontology. Dr Trombelli also maintains a private practice limited to periodontology and oral surgery.





 Treatment Planning in Restorative Dentistry and Implant Prosthodontics
Treatment Planning in Restorative Dentistry and Implant Prosthodontics Fundamentals of Treatment Planning: Guidelines on How to Develop, Plan, Write, and Deliver a Prosthodontic Care Project
Fundamentals of Treatment Planning: Guidelines on How to Develop, Plan, Write, and Deliver a Prosthodontic Care Project